Myelodysplasia, also known as myelodysplastic syndromes (MDS), is a group of disorders caused by poorly formed or dysfunctional blood cells. These conditions arise when the bone marrow, responsible for producing blood cells, doesn't function correctly. Symptoms can vary but often include fatigue, shortness of breath, easy bruising, and frequent infections. Diagnosis typically involves blood tests, bone marrow exams, and genetic testing. Treatment options range from supportive care to more aggressive approaches like chemotherapy or stem cell transplants. Understanding myelodysplasia is crucial for managing the disease and improving quality of life. Let's dive into 50 essential facts about this complex condition.
Key Takeaways:
- Myelodysplasia, or MDS, disrupts blood cell production and can progress to leukemia. It's more common in older adults and is diagnosed through blood tests and bone marrow biopsies.
- While there's no cure for MDS, treatments like supportive care, growth factors, and stem cell transplants can help manage symptoms and improve quality of life. Regular monitoring and lifestyle adjustments are crucial for living with MDS.
Understanding Myelodysplasia
Myelodysplasia, also known as myelodysplastic syndromes (MDS), is a group of disorders caused by poorly formed or dysfunctional blood cells. These conditions can be complex, so let's break down some key facts.
-
Myelodysplasia affects the bone marrow. The bone marrow is where blood cells are produced, and in MDS, this process is disrupted.
-
There are different types of MDS. These types are classified based on which blood cells are affected and how severe the abnormalities are.
-
MDS can progress to leukemia. In some cases, MDS can evolve into acute myeloid leukemia (AML), a more aggressive form of cancer.
-
Symptoms can be subtle. Early signs might include fatigue, shortness of breath, or frequent infections, often mistaken for other conditions.
-
MDS is more common in older adults. Most cases are diagnosed in people over the age of 60.
-
Genetic mutations play a role. Certain genetic changes can increase the risk of developing MDS.
-
Exposure to chemicals can be a risk factor. Long-term exposure to chemicals like benzene has been linked to MDS.
-
Previous cancer treatments can increase risk. Chemotherapy and radiation therapy can damage bone marrow, leading to MDS.
-
MDS is diagnosed through blood tests and bone marrow biopsies. These tests help determine the type and severity of the disorder.
-
There is no cure for MDS. Treatment focuses on managing symptoms and improving quality of life.
Symptoms and Diagnosis
Recognizing the symptoms and understanding the diagnostic process is crucial for managing MDS effectively.
-
Anemia is a common symptom. This can cause fatigue, weakness, and pale skin.
-
Frequent infections may occur. Due to low white blood cell counts, patients are more susceptible to infections.
-
Easy bruising and bleeding. Low platelet counts can lead to bruising and prolonged bleeding from minor cuts.
-
Bone pain can be a symptom. Some patients experience pain in their bones or joints.
-
Routine blood tests can reveal abnormalities. Unusual results in a complete blood count (CBC) can prompt further investigation.
-
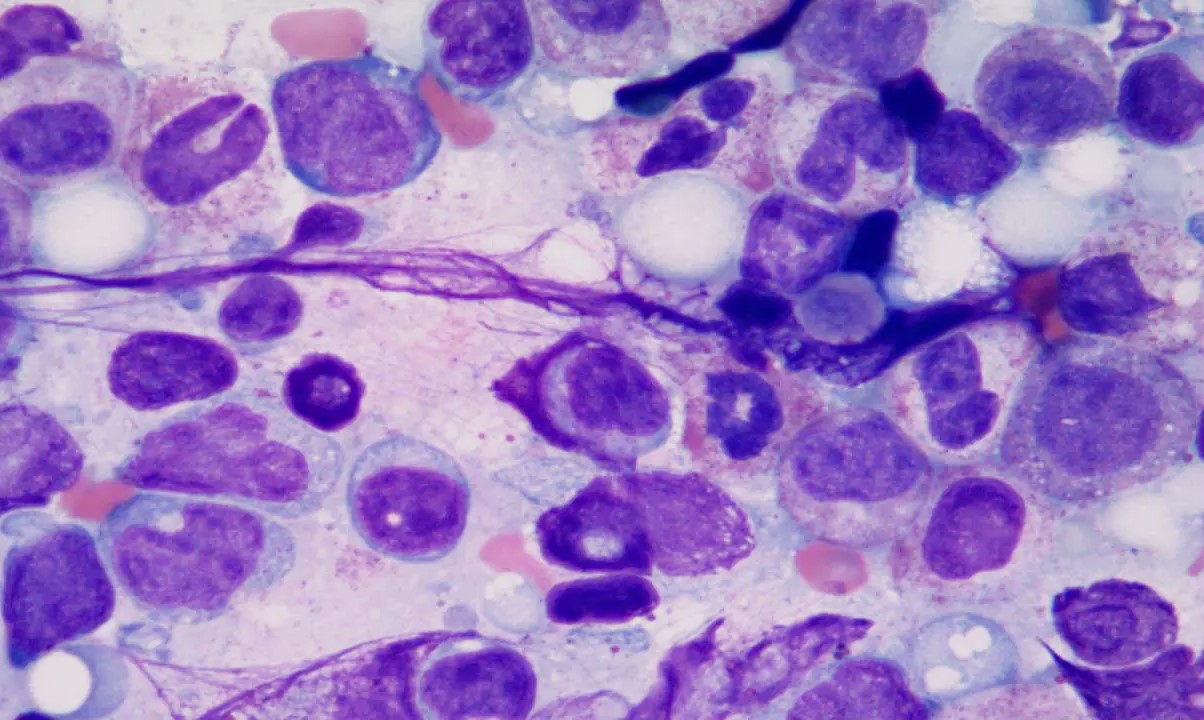
Bone marrow biopsy is definitive. This procedure involves taking a small sample of bone marrow to examine under a microscope.
-
Cytogenetic analysis helps identify genetic abnormalities. This test looks for changes in chromosomes that are common in MDS.
-
Flow cytometry can be used. This technique analyzes the characteristics of blood cells to help diagnose MDS.
-
MDS can be classified into subtypes. The World Health Organization (WHO) classification system is commonly used.
-
Prognosis varies widely. Factors like age, overall health, and specific genetic mutations influence outcomes.
Treatment Options
While there is no cure, various treatments can help manage symptoms and improve quality of life for those with MDS.
-
Supportive care is essential. This includes blood transfusions and medications to manage symptoms.
-
Growth factors can stimulate blood cell production. Drugs like erythropoietin can help increase red blood cell counts.
-
Chemotherapy may be used. Low-dose chemotherapy can help control the disease in some patients.
-
Immunosuppressive therapy is an option. Drugs that suppress the immune system can be effective for certain types of MDS.
-
Stem cell transplant offers potential for cure. This procedure replaces damaged bone marrow with healthy cells from a donor.
-
Clinical trials provide access to new treatments. Patients can participate in studies testing innovative therapies.
-
Lenalidomide is used for specific subtypes. This drug is particularly effective for MDS with a specific genetic abnormality.
-
Hypomethylating agents can be beneficial. Drugs like azacitidine and decitabine help control abnormal cell growth.
-
Iron chelation therapy may be needed. Frequent blood transfusions can lead to iron overload, requiring treatment to remove excess iron.
-
Regular monitoring is crucial. Ongoing blood tests and check-ups help track disease progression and treatment effectiveness.
Living with Myelodysplasia
Managing daily life with MDS involves understanding the condition and making lifestyle adjustments.
-
Nutrition plays a role. A balanced diet can help maintain overall health and energy levels.
-
Exercise can improve well-being. Regular physical activity, tailored to individual capabilities, can boost mood and stamina.
-
Infection prevention is important. Good hygiene and avoiding sick contacts can reduce infection risk.
-
Emotional support is vital. Counseling or support groups can help patients and families cope with the emotional impact of MDS.
-
Medication adherence is key. Taking prescribed medications as directed is crucial for managing symptoms.
-
Regular follow-ups are necessary. Consistent medical appointments ensure timely adjustments to treatment plans.
-
Understanding treatment side effects helps. Being aware of potential side effects allows for better management and communication with healthcare providers.
-
Financial planning may be needed. Treatment costs can be high, so planning and seeking financial assistance can be beneficial.
-
Advance care planning is wise. Discussing future healthcare preferences with loved ones and healthcare providers ensures wishes are respected.
-
Staying informed empowers patients. Keeping up-to-date with the latest research and treatment options helps patients make informed decisions.
Research and Future Directions
Ongoing research aims to improve understanding and treatment of MDS, offering hope for the future.
-
Genetic research is advancing. Studies on genetic mutations and their impact on MDS are ongoing.
-
New drug development is promising. Researchers are working on novel therapies to target specific aspects of MDS.
-
Immunotherapy is being explored. Treatments that harness the immune system to fight MDS are under investigation.
-
Personalized medicine is a goal. Tailoring treatments to individual genetic profiles could improve outcomes.
-
Stem cell research offers potential. Advances in stem cell technology may lead to new treatment options.
-
International collaboration is key. Researchers worldwide are working together to share knowledge and resources.
-
Patient registries help track outcomes. Collecting data from MDS patients helps researchers understand the disease better.
-
Public awareness is increasing. Efforts to educate the public about MDS are helping to reduce stigma and improve support.
-
Advocacy groups provide support. Organizations dedicated to MDS offer resources and advocacy for patients and families.
-
Hope for the future. Continued research and advancements in treatment offer hope for better outcomes for those with MDS.
Final Thoughts on Myelodysplasia
Myelodysplasia, often called MDS, is a complex condition affecting blood cell production. Understanding its symptoms, causes, and treatments can make a big difference in managing the disease. Early detection is key, so regular check-ups and being aware of changes in your health are crucial. Treatments range from medications to bone marrow transplants, depending on the severity.
Staying informed and working closely with healthcare providers can help navigate the challenges of MDS. Support groups and resources are available for patients and families, offering valuable information and emotional support.
Remember, while MDS can be serious, advancements in medical research continue to improve outcomes. Stay proactive, seek support, and maintain open communication with your medical team. Knowledge is power when dealing with myelodysplasia.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
