Vancomycin-Resistant Enterococcus (VRE) is a type of bacteria that has developed resistance to the antibiotic vancomycin, making infections difficult to treat. VRE primarily affects individuals with weakened immune systems, such as hospital patients or those undergoing treatments like chemotherapy. Understanding VRE is crucial because it can lead to severe infections, including bloodstream infections, urinary tract infections, and wound infections. This post will provide 40 essential facts about VRE, covering its causes, symptoms, treatment options, and prevention strategies. By the end, you'll have a comprehensive understanding of this resistant bacterium and how to protect yourself and others from its impact.
Key Takeaways:
- VRE is a tough bacteria that resists antibiotics, causing tricky infections. Preventing spread through handwashing and infection control is crucial for healthcare safety.
- VRE impacts patients, healthcare workers, and healthcare systems worldwide. Research and global collaboration are essential to combat this global health concern.
What is Vancomycin-Resistant Enterococcus (VRE)?
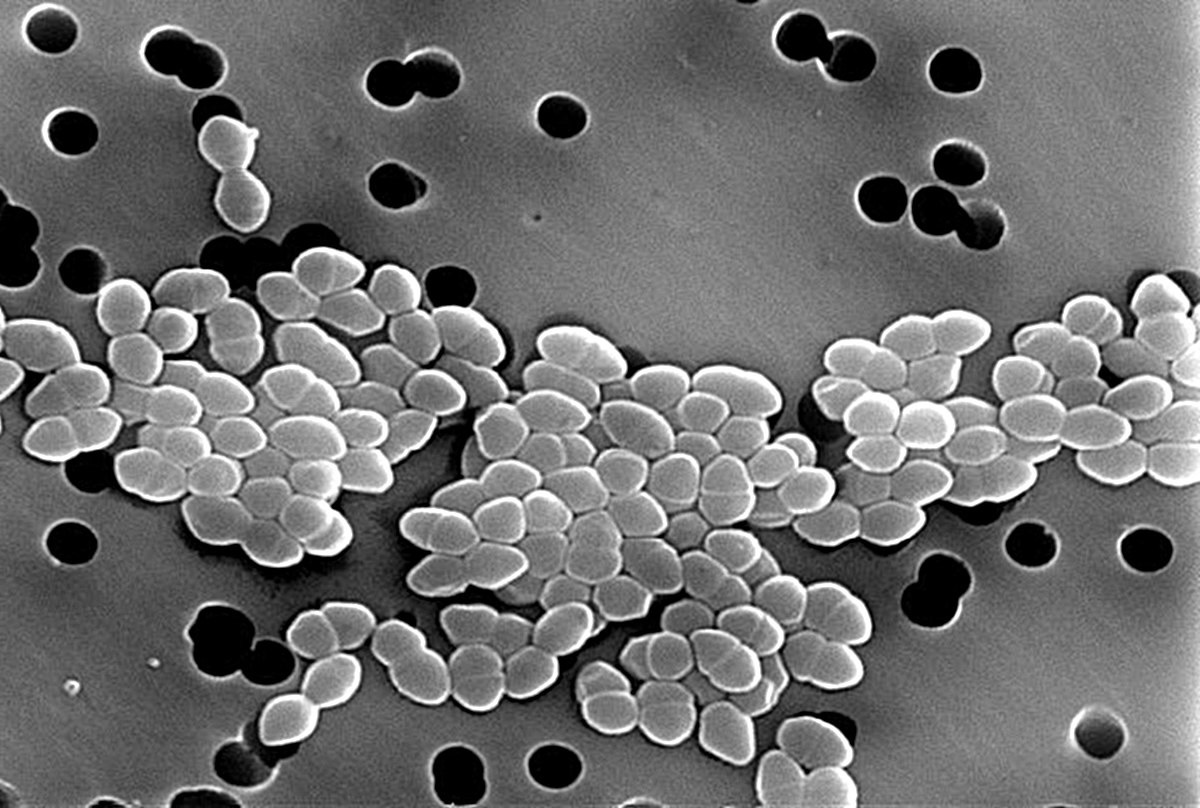
Vancomycin-Resistant Enterococcus (VRE) is a type of bacteria that has become resistant to the antibiotic vancomycin. This resistance makes infections difficult to treat. VRE is a significant concern in healthcare settings.
- VRE is a type of Enterococcus bacteria that has developed resistance to vancomycin, an antibiotic often used to treat serious infections.
- Enterococcus bacteria are normally found in the human intestines and the female genital tract. They usually do not cause harm in healthy individuals.
- VRE can cause a variety of infections, including urinary tract infections, bloodstream infections, and wound infections.
- The resistance to vancomycin makes VRE infections particularly challenging to treat, often requiring alternative antibiotics.
How Does VRE Spread?
Understanding how VRE spreads is crucial for preventing infections. VRE can be transmitted in several ways, especially in healthcare environments.
- VRE spreads through direct contact with contaminated surfaces or hands. It does not spread through the air like some other infections.
- Healthcare workers can inadvertently transfer VRE from one patient to another if proper hygiene practices are not followed.
- Patients with weakened immune systems are more susceptible to VRE infections, making it a significant concern in hospitals and long-term care facilities.
- VRE can survive on surfaces for extended periods, increasing the risk of transmission in healthcare settings.
Symptoms of VRE Infections
Recognizing the symptoms of VRE infections can help in early diagnosis and treatment. Symptoms vary depending on the type of infection.
- Urinary tract infections caused by VRE may present symptoms such as a strong urge to urinate, a burning sensation during urination, and cloudy or bloody urine.
- Bloodstream infections (bacteremia) due to VRE can cause fever, chills, and low blood pressure. These infections can be life-threatening.
- Wound infections from VRE may result in redness, swelling, and pus at the site of the wound.
- VRE can also cause endocarditis, an infection of the heart valves, which presents symptoms like fever, fatigue, and heart murmurs.
Diagnosing VRE
Accurate diagnosis is essential for managing VRE infections. Several methods are used to identify the presence of VRE.
- Laboratory tests are required to diagnose VRE. These tests involve culturing samples from the infected area.
- Polymerase chain reaction (PCR) tests can detect the genetic material of VRE, providing a quicker diagnosis than traditional culture methods.
- Antibiotic susceptibility testing helps determine which antibiotics are effective against the specific strain of VRE.
- Screening for VRE may be conducted in healthcare settings, especially for patients at high risk of infection.
Treatment Options for VRE
Treating VRE infections can be challenging due to antibiotic resistance. However, several treatment options are available.
- Alternative antibiotics such as linezolid, daptomycin, and tigecycline may be used to treat VRE infections.
- Combination antibiotic therapy might be necessary to effectively combat VRE.
- Supportive care is crucial for managing symptoms and preventing complications in patients with VRE infections.
- In some cases, surgical intervention may be required to remove infected tissue or devices.
Preventing VRE Infections
Prevention is key to controlling the spread of VRE. Several strategies can help reduce the risk of infection.
- Hand hygiene is the most effective way to prevent the spread of VRE. Regular handwashing with soap and water or using alcohol-based hand sanitizers is essential.
- Healthcare facilities should implement strict infection control measures, including isolating patients with VRE and using personal protective equipment (PPE).
- Environmental cleaning and disinfection are crucial in healthcare settings to eliminate VRE from surfaces.
- Antibiotic stewardship programs aim to reduce the overuse and misuse of antibiotics, which can help prevent the development of antibiotic-resistant bacteria like VRE.
The Impact of VRE on Healthcare
VRE poses significant challenges for healthcare systems. Its impact extends beyond individual patients to the broader healthcare environment.
- VRE infections can lead to longer hospital stays, increasing healthcare costs and resource utilization.
- The presence of VRE in a healthcare facility can result in outbreaks, requiring extensive infection control measures.
- Patients with VRE infections may experience more severe outcomes, including higher mortality rates compared to those with non-resistant infections.
- Healthcare workers face increased stress and workload when managing VRE infections, impacting overall healthcare delivery.
Research and Future Directions
Ongoing research is essential to combat VRE and develop new treatment strategies. Scientists are exploring various avenues to address this issue.
- New antibiotics are being developed to target VRE and other antibiotic-resistant bacteria.
- Research into alternative therapies, such as bacteriophage therapy, is ongoing and shows promise in treating VRE infections.
- Genomic studies of VRE aim to understand the mechanisms of resistance and identify potential targets for new treatments.
- Vaccines against VRE are being investigated as a potential preventive measure.
Global Perspective on VRE
VRE is a global health concern, with varying prevalence and challenges in different regions. Understanding the global perspective can inform better strategies.
- VRE prevalence varies worldwide, with higher rates reported in some countries due to differences in antibiotic use and infection control practices.
- International collaboration is crucial for addressing the spread of VRE, as bacteria do not recognize borders.
- Global surveillance programs monitor the spread of VRE and other antibiotic-resistant bacteria, providing valuable data for public health efforts.
- Education and awareness campaigns are essential to inform healthcare professionals and the public about the risks and prevention of VRE.
Personal Stories and Experiences
Hearing from those affected by VRE can provide valuable insights and highlight the human impact of this issue.
- Patients who have battled VRE infections often share stories of prolonged hospital stays, multiple treatments, and the emotional toll of dealing with a resistant infection.
- Healthcare workers on the front lines face challenges in managing VRE, from implementing strict infection control measures to providing compassionate care to affected patients.
- Families of patients with VRE experience stress and anxiety, emphasizing the importance of support systems during treatment and recovery.
- Survivors of VRE infections often advocate for better infection control practices and increased research funding to combat antibiotic resistance.
The Final Word on Vancomycin-Resistant Enterococcus
Vancomycin-Resistant Enterococcus (VRE) poses a serious threat to public health. This superbug resists many antibiotics, making infections tough to treat. Hospitals and healthcare settings see the highest rates of VRE, often affecting patients with weakened immune systems. Proper hygiene, strict infection control measures, and prudent antibiotic use can help curb its spread. Researchers continue to seek new treatments and strategies to combat VRE. Awareness and education play crucial roles in preventing infections. By understanding VRE, we can better protect ourselves and our communities. Stay informed, practice good hygiene, and support efforts to develop new antibiotics. Together, we can tackle this challenge and safeguard public health.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
