Hereditary pancreatitis is a rare genetic condition that causes inflammation of the pancreas. This condition often starts in childhood and can lead to chronic pain, digestive issues, and an increased risk of pancreatic cancer. What causes hereditary pancreatitis? Mutations in specific genes, such as PRSS1, are the primary culprits. These genetic changes cause the pancreas to become inflamed more easily. How is it diagnosed? Doctors use a combination of family history, genetic testing, and imaging studies. Can it be treated? While there's no cure, treatments focus on managing symptoms and preventing complications. Understanding hereditary pancreatitis can help those affected lead healthier lives.
Key Takeaways:
- Hereditary Pancreatitis is a rare genetic condition causing severe abdominal pain and complications. Early diagnosis, pain management, and genetic counseling are crucial for affected individuals and their families.
- Ongoing research aims to improve understanding and treatment of Hereditary Pancreatitis. Lifestyle adjustments, regular monitoring, and raising awareness can enhance the quality of life for those affected by this condition.
What is Hereditary Pancreatitis?
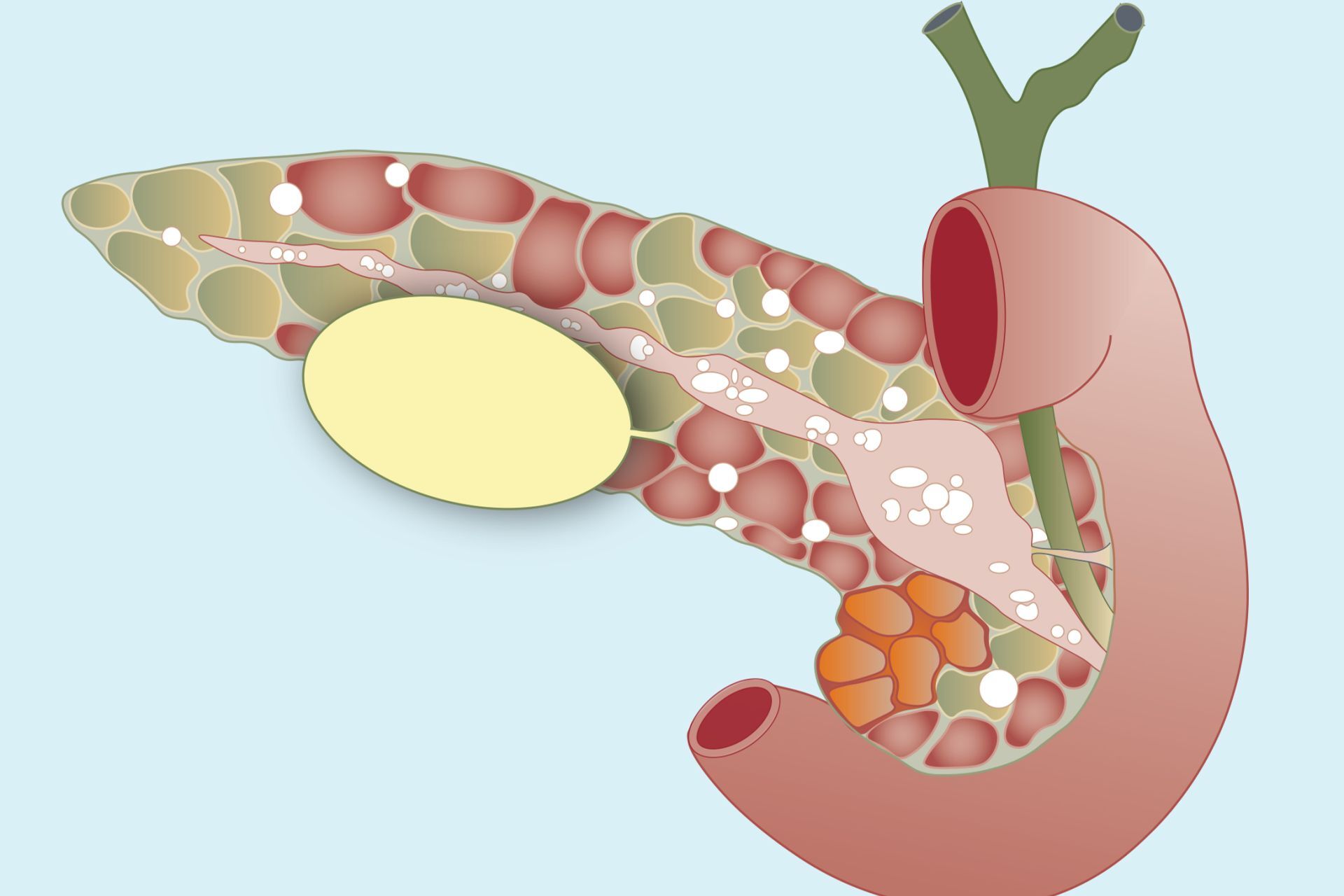
Hereditary Pancreatitis (HP) is a rare genetic condition that affects the pancreas. It leads to recurrent episodes of inflammation, causing severe abdominal pain and other complications. Here are some intriguing facts about this condition.
-
Genetic Mutation: HP is caused by mutations in the PRSS1 gene. This gene provides instructions for making an enzyme called trypsinogen, which is crucial for digestion.
-
Autosomal Dominant: The condition is inherited in an autosomal dominant pattern. This means only one copy of the altered gene is sufficient to cause the disorder.
-
Early Onset: Symptoms often appear in childhood or adolescence, typically before the age of 20.
-
Recurrent Episodes: Individuals with HP experience recurrent episodes of pancreatitis, which can be extremely painful.
-
Chronic Inflammation: Over time, repeated inflammation can lead to chronic pancreatitis, causing permanent damage to the pancreas.
Symptoms and Diagnosis
Recognizing the symptoms early can lead to better management of the condition. Here are some key facts about the symptoms and diagnosis of HP.
-
Severe Abdominal Pain: The most common symptom is severe abdominal pain, often radiating to the back.
-
Nausea and Vomiting: During an episode, individuals may experience nausea and vomiting.
-
Weight Loss: Chronic pancreatitis can lead to weight loss due to malabsorption of nutrients.
-
Diabetes Risk: Damage to the pancreas can impair insulin production, increasing the risk of diabetes.
-
Diagnostic Tests: Blood tests, imaging studies like CT scans, and genetic testing are used to diagnose HP.
Treatment and Management
Managing HP involves addressing symptoms and preventing complications. Here are some important facts about treatment and management.
-
Pain Management: Pain relief is a primary focus, often requiring medications or nerve blocks.
-
Enzyme Supplements: Pancreatic enzyme supplements help with digestion and nutrient absorption.
-
Dietary Changes: A low-fat diet can reduce the frequency of pancreatitis episodes.
-
Avoiding Alcohol: Alcohol can exacerbate symptoms and should be avoided.
-
Surgery: In severe cases, surgical options like pancreatectomy may be considered.
Complications and Risks
HP can lead to several complications, impacting overall health. Here are some critical facts about the risks associated with HP.
-
Pancreatic Cancer: Individuals with HP have an increased risk of developing pancreatic cancer.
-
Pseudocysts: Fluid-filled sacs called pseudocysts can form in the pancreas, causing pain and infection.
-
Malnutrition: Chronic pancreatitis can lead to malnutrition due to poor absorption of nutrients.
-
Bile Duct Obstruction: Inflammation can block the bile duct, leading to jaundice and liver problems.
-
Infection: Pancreatic tissue can become infected, requiring antibiotics or drainage procedures.
Genetic Counseling and Family Planning
Given the hereditary nature of HP, genetic counseling is crucial for affected families. Here are some facts about genetic counseling and family planning.
-
Genetic Testing: Testing can identify carriers of the PRSS1 mutation, helping with early diagnosis and management.
-
Family Screening: Relatives of affected individuals may also undergo genetic testing to determine their risk.
-
Prenatal Testing: Prenatal genetic testing can identify the mutation in unborn children.
-
Reproductive Options: Families may consider reproductive options like IVF with genetic screening to prevent passing on the mutation.
-
Support Groups: Joining support groups can provide emotional support and valuable information for families dealing with HP.
Research and Future Directions
Ongoing research aims to improve understanding and treatment of HP. Here are some exciting facts about current research and future directions.
-
Gene Therapy: Researchers are exploring gene therapy as a potential treatment for HP.
-
New Medications: Development of new medications to reduce inflammation and pain is underway.
-
Biomarkers: Identifying biomarkers can help in early diagnosis and monitoring of the disease.
-
Stem Cell Research: Stem cell research holds promise for regenerating damaged pancreatic tissue.
-
Clinical Trials: Participation in clinical trials can provide access to cutting-edge treatments and contribute to scientific knowledge.
Living with Hereditary Pancreatitis
Living with HP requires ongoing management and lifestyle adjustments. Here are some practical facts about daily life with HP.
-
Regular Monitoring: Regular check-ups and monitoring are essential to manage the condition effectively.
-
Pain Management Techniques: Techniques like meditation, yoga, and acupuncture can help manage pain.
-
Nutritional Support: Working with a nutritionist can ensure adequate nutrient intake and prevent malnutrition.
-
Mental Health: Chronic illness can impact mental health, making psychological support important.
-
Exercise: Regular, moderate exercise can improve overall health and well-being.
Awareness and Advocacy
Raising awareness about HP can lead to better support and resources for affected individuals. Here are some facts about awareness and advocacy efforts.
-
Awareness Campaigns: Campaigns and events can educate the public and healthcare professionals about HP.
-
Advocacy Groups: Organizations advocate for research funding and support services for those with HP.
-
Educational Materials: Providing educational materials can help patients and families understand the condition better.
-
Policy Changes: Advocacy can lead to policy changes that improve access to care and support for individuals with HP.
-
Community Support: Building a strong community of patients, families, and healthcare providers can enhance the quality of life for those affected by HP.
Final Thoughts on Hereditary Pancreatitis
Hereditary pancreatitis is a rare but serious condition. It’s caused by genetic mutations passed down through families. Symptoms often start in childhood and can include severe abdominal pain, nausea, and vomiting. Over time, chronic inflammation can lead to complications like diabetes and pancreatic cancer. Early diagnosis and management are crucial for improving quality of life. Treatments focus on pain relief, enzyme supplements, and lifestyle changes. Genetic counseling can help families understand their risks and options. Awareness and education about this condition are essential for early intervention and better outcomes. If you or a loved one show symptoms, consult a healthcare provider for proper evaluation and care. Understanding hereditary pancreatitis empowers patients and families to take proactive steps in managing this challenging condition.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
