Eosinophilic myocarditis is a rare but serious condition where a type of white blood cell called eosinophils infiltrates the heart muscle, causing inflammation. This can lead to symptoms like chest pain, shortness of breath, and even heart failure. Eosinophilic myocarditis can be triggered by various factors, including infections, medications, and autoimmune diseases. Diagnosing this condition often requires a combination of blood tests, imaging studies, and sometimes a heart biopsy. Treatment typically involves addressing the underlying cause and may include medications like corticosteroids to reduce inflammation. Understanding this condition is crucial for timely intervention and better outcomes.
Key Takeaways:
- Eosinophilic myocarditis is a rare heart condition caused by an increase in white blood cells. Early detection and treatment are crucial for a better prognosis and long-term management.
- Lifestyle adjustments, regular medical check-ups, and emotional support are essential for individuals living with eosinophilic myocarditis. Staying informed about the latest research and treatment options can empower patients to take an active role in their care.
What is Eosinophilic Myocarditis?
Eosinophilic myocarditis is a rare type of heart inflammation caused by an increased number of eosinophils, a type of white blood cell. This condition can lead to severe heart problems if not treated promptly. Here are some fascinating facts about eosinophilic myocarditis.
-
Eosinophils are a type of white blood cell that play a crucial role in the body's immune response, particularly in fighting off parasitic infections and allergic reactions.
-
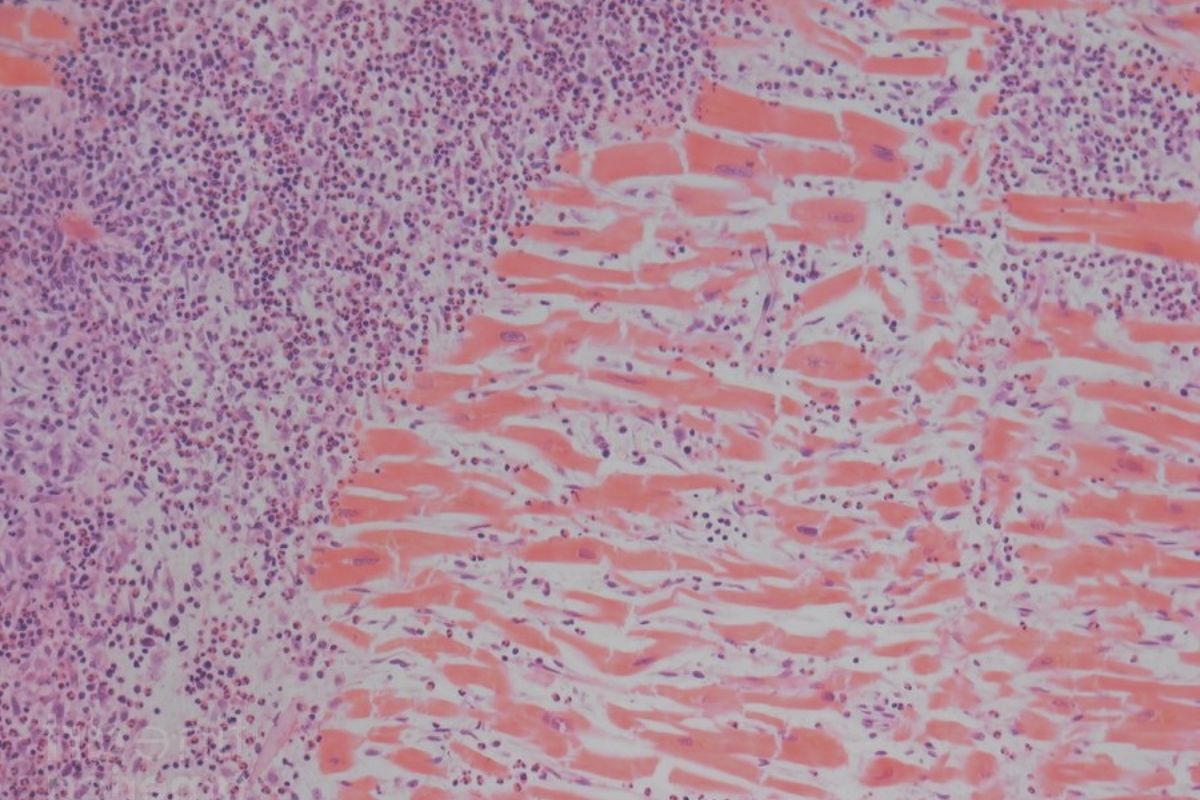
Eosinophilic myocarditis occurs when these eosinophils infiltrate the heart muscle, causing inflammation and damage.
-
This condition can be triggered by various factors, including infections, medications, and autoimmune diseases.
-
Symptoms of eosinophilic myocarditis can include chest pain, shortness of breath, fatigue, and palpitations.
-
In severe cases, eosinophilic myocarditis can lead to heart failure or sudden cardiac death.
Causes and Risk Factors
Understanding what causes eosinophilic myocarditis and the risk factors involved can help in early detection and treatment.
-
Parasitic infections, such as those caused by Toxocara or Trichinella, can lead to eosinophilic myocarditis.
-
Certain medications, including antibiotics and anti-seizure drugs, have been linked to this condition.
-
Autoimmune diseases, like Churg-Strauss syndrome, can also cause eosinophilic myocarditis.
-
Hypereosinophilic syndrome, a condition characterized by an abnormally high number of eosinophils, is another risk factor.
-
Some cases of eosinophilic myocarditis are idiopathic, meaning the cause is unknown.
Diagnosis and Detection
Early diagnosis is crucial for effective treatment of eosinophilic myocarditis. Here are some methods used to detect this condition.
-
Blood tests can reveal elevated levels of eosinophils, which may indicate eosinophilic myocarditis.
-
An electrocardiogram (ECG) can detect abnormal heart rhythms associated with this condition.
-
Echocardiography uses ultrasound waves to create images of the heart, helping to identify inflammation and damage.
-
Cardiac MRI provides detailed images of the heart's structure and can detect areas of inflammation.
-
Endomyocardial biopsy, where a small sample of heart tissue is taken for examination, is the definitive test for diagnosing eosinophilic myocarditis.
Treatment Options
Once diagnosed, various treatment options are available to manage eosinophilic myocarditis.
-
Corticosteroids are often the first line of treatment, as they help reduce inflammation.
-
Immunosuppressive drugs may be used in cases where corticosteroids are not effective.
-
Treating the underlying cause, such as discontinuing a medication or treating an infection, is crucial.
-
In severe cases, heart failure medications may be needed to manage symptoms.
-
Regular follow-up with a cardiologist is essential to monitor the condition and adjust treatment as needed.
Prognosis and Long-Term Outlook
The long-term outlook for individuals with eosinophilic myocarditis can vary widely based on several factors.
-
Early diagnosis and treatment significantly improve the prognosis for most patients.
-
Some individuals may experience a complete recovery with appropriate treatment.
-
Others may develop chronic heart issues, requiring ongoing medical management.
-
Regular monitoring and follow-up care are essential to detect any recurrence or complications.
-
Advances in medical research continue to improve the understanding and treatment of eosinophilic myocarditis.
Interesting Facts and Statistics
Here are some additional interesting facts and statistics about eosinophilic myocarditis.
-
Eosinophilic myocarditis is considered a rare condition, with an estimated incidence of less than 0.5% in the general population.
-
Men are slightly more likely to develop eosinophilic myocarditis than women.
-
The condition can occur at any age but is most commonly diagnosed in middle-aged adults.
-
Eosinophilic myocarditis can mimic other heart conditions, making accurate diagnosis challenging.
-
Research is ongoing to better understand the genetic and environmental factors that contribute to eosinophilic myocarditis.
Living with Eosinophilic Myocarditis
Managing life with eosinophilic myocarditis involves several lifestyle adjustments and ongoing medical care.
-
Patients are often advised to avoid strenuous physical activity to reduce stress on the heart.
-
A heart-healthy diet, rich in fruits, vegetables, and whole grains, can support overall cardiovascular health.
-
Regular medical check-ups are crucial to monitor heart function and adjust treatment as needed.
-
Emotional support from family, friends, or support groups can help individuals cope with the challenges of living with a chronic condition.
-
Staying informed about the latest research and treatment options can empower patients to take an active role in their care.
Research and Future Directions
Ongoing research aims to improve the understanding and treatment of eosinophilic myocarditis.
-
Scientists are investigating the genetic factors that may predispose individuals to eosinophilic myocarditis.
-
New medications and treatment approaches are being developed to target the underlying causes of the condition.
-
Advances in imaging technology are improving the ability to detect and monitor eosinophilic myocarditis.
-
Collaborative research efforts are helping to identify biomarkers that could lead to earlier diagnosis and more personalized treatment.
-
Increased awareness and education about eosinophilic myocarditis can lead to better outcomes for patients worldwide.
Final Thoughts on Eosinophilic Myocarditis
Eosinophilic myocarditis, though rare, demands attention due to its serious implications. Understanding its symptoms, causes, and treatments can make a significant difference in managing this condition. Early detection often leads to better outcomes, so staying informed is crucial. Remember, symptoms like chest pain, shortness of breath, or unexplained fatigue shouldn't be ignored. Consulting a healthcare professional at the first sign of trouble can be life-saving.
Treatment options vary, ranging from medications to manage inflammation to more intensive therapies for severe cases. Awareness and education about eosinophilic myocarditis can empower patients and caregivers alike. By staying vigilant and proactive, you can navigate this challenging condition more effectively. Knowledge truly is power when it comes to health. Stay informed, stay healthy.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
