What is Ventricular Fibrillation? It's a serious heart rhythm problem that can be life-threatening. This condition happens when the heart's lower chambers, called ventricles, quiver instead of pumping blood effectively. This chaotic heartbeat can lead to sudden cardiac arrest, where the heart stops beating altogether. Without immediate treatment, it can be fatal within minutes. Why does it matter? Understanding ventricular fibrillation is crucial because it requires quick action, often involving CPR and defibrillation, to restore a normal heart rhythm. Recognizing symptoms like sudden collapse, no pulse, or loss of consciousness can save lives. Who is at risk? People with heart disease, previous heart attacks, or genetic conditions may be more susceptible. Knowing these facts can help in preventing and managing this critical condition. Stay informed to protect yourself and others from this silent threat.
Key Takeaways:
- Ventricular fibrillation is a serious heart condition that requires immediate medical intervention. It can occur suddenly without warning signs, and knowing the risk factors can help in prevention and early detection.
- Advanced technology, lifestyle changes, and support networks play a crucial role in managing ventricular fibrillation. With prompt treatment and awareness, many people can survive and lead fulfilling lives post-VF.
Understanding Ventricular Fibrillation
Ventricular fibrillation (VF) is a serious heart condition that can be life-threatening. It involves rapid, erratic electrical impulses in the heart's ventricles, causing them to quiver instead of pumping blood. Let's explore some intriguing facts about this condition.
-
VF is a Medical Emergency
When VF occurs, blood isn't effectively pumped to the body, leading to a sudden cardiac arrest. Immediate medical intervention is crucial. -
Causes of VF
Heart attacks, cardiomyopathy, and electrolyte imbalances are common triggers. Sometimes, it happens without any known cause. -
Symptoms are Sudden
Symptoms include sudden collapse, loss of consciousness, and no pulse. There might be no warning signs. -
Defibrillation is Key
An automated external defibrillator (AED) can restore a normal heartbeat. Quick use of an AED increases survival chances. -
CPR Can Help
Cardiopulmonary resuscitation (CPR) keeps blood flowing to vital organs until defibrillation can be performed.
Risk Factors for Ventricular Fibrillation
Certain factors can increase the likelihood of experiencing VF. Knowing these can help in prevention and early detection.
-
Previous Heart Attack
A history of heart attacks raises the risk of VF due to damaged heart tissue. -
Heart Disease
Conditions like coronary artery disease and cardiomyopathy are significant risk factors. -
Genetic Predisposition
Some people inherit conditions that make them more susceptible to VF. -
Substance Abuse
Drugs like cocaine and methamphetamine can trigger VF. -
Electrolyte Imbalances
Low potassium or magnesium levels can lead to VF.
Diagnosing Ventricular Fibrillation
Accurate diagnosis is essential for effective treatment. Here are some methods used to identify VF.
-
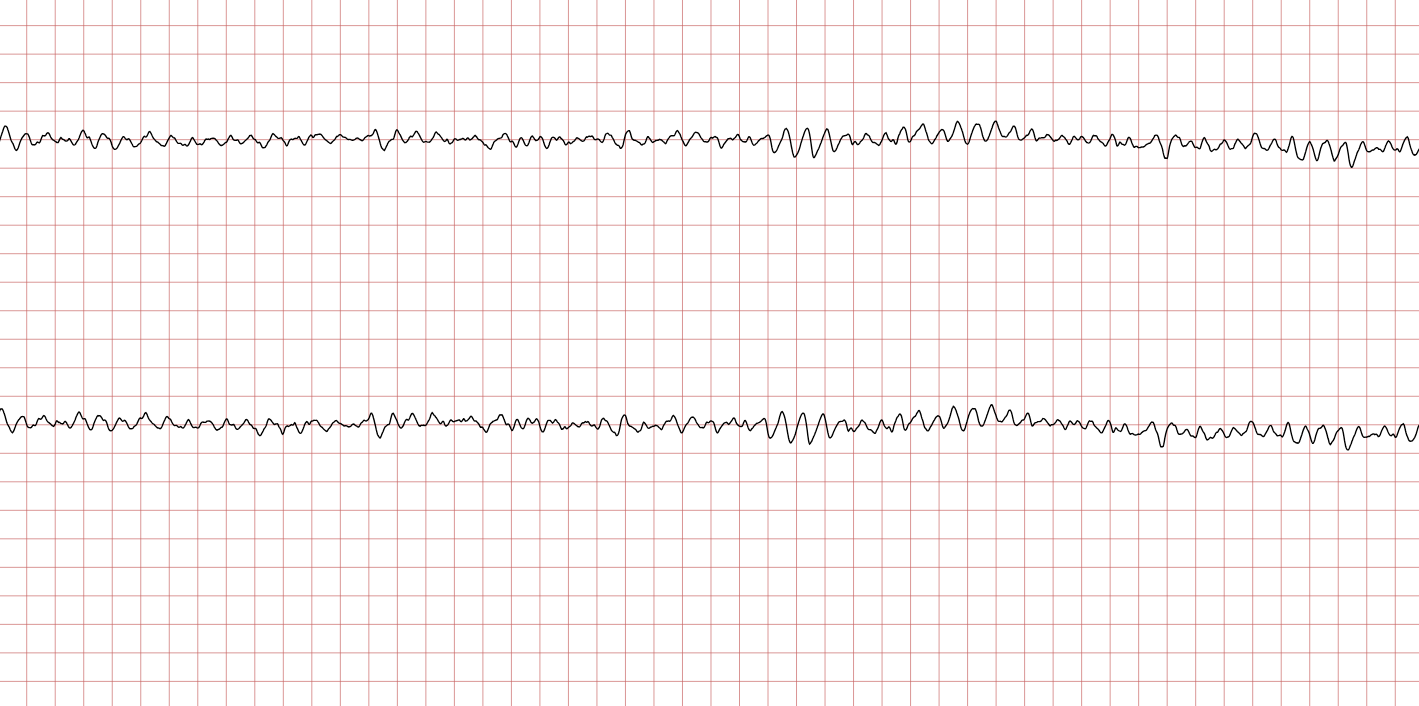
Electrocardiogram (ECG)
An ECG records the heart's electrical activity and can detect VF. -
Blood Tests
These can identify electrolyte imbalances or heart damage. -
Echocardiogram
This ultrasound test shows the heart's structure and function. -
Coronary Angiography
This test checks for blockages in the coronary arteries. -
Holter Monitor
A portable ECG device worn for a day or more to monitor heart rhythms.
Treatment Options for Ventricular Fibrillation
Treating VF involves immediate and long-term strategies to prevent recurrence.
-
Immediate Defibrillation
The most effective immediate treatment for VF is defibrillation. -
Medications
Drugs like beta-blockers and antiarrhythmics help manage heart rhythms. -
Implantable Cardioverter-Defibrillator (ICD)
An ICD monitors heart rhythms and delivers shocks to correct VF. -
Lifestyle Changes
Diet, exercise, and quitting smoking can reduce VF risk. -
Surgical Procedures
In some cases, surgery may be needed to correct underlying heart issues.
Prevention of Ventricular Fibrillation
Preventing VF involves managing risk factors and maintaining heart health.
-
Regular Check-Ups
Routine medical exams can detect heart problems early. -
Healthy Diet
A diet low in saturated fats and high in fruits and vegetables supports heart health. -
Exercise Regularly
Physical activity strengthens the heart and improves circulation. -
Avoid Smoking
Smoking damages blood vessels and increases VF risk. -
Limit Alcohol
Excessive alcohol can lead to heart problems, including VF.
The Role of Technology in Managing VF
Advancements in technology have improved the management and treatment of VF.
-
Wearable Devices
Smartwatches and fitness trackers can monitor heart rates and detect irregularities. -
Telemedicine
Remote consultations allow for continuous monitoring and quick intervention. -
Advanced Imaging Techniques
MRI and CT scans provide detailed images of the heart. -
Genetic Testing
Identifies individuals at risk due to inherited conditions. -
Mobile Apps
Apps help track symptoms and medication schedules.
Impact of Ventricular Fibrillation on Daily Life
Living with VF requires adjustments and awareness to manage the condition effectively.
-
Medication Adherence
Taking prescribed medications regularly is crucial. -
Emergency Preparedness
Knowing CPR and having an AED nearby can save lives. -
Stress Management
Reducing stress through relaxation techniques benefits heart health. -
Support Networks
Family and friends provide emotional and practical support. -
Regular Monitoring
Keeping track of heart health helps in early detection of issues.
Research and Future Directions
Ongoing research aims to improve VF treatment and prevention strategies.
-
Gene Therapy
Investigating ways to correct genetic mutations causing VF. -
Stem Cell Research
Exploring the potential of stem cells to repair damaged heart tissue. -
New Medications
Developing drugs that target specific pathways involved in VF. -
Improved Defibrillators
Creating more efficient and user-friendly defibrillation devices. -
Public Awareness Campaigns
Educating the public about VF and its symptoms.
Myths and Misconceptions about Ventricular Fibrillation
Clearing up common misunderstandings can lead to better awareness and response.
-
VF is Not a Heart Attack
Although related, VF and heart attacks are different conditions. -
Only Older Adults are Affected
VF can occur at any age, though risk increases with age. -
VF Always Shows Symptoms
Sometimes, VF occurs without noticeable symptoms. -
CPR Alone Can Save Lives
While crucial, CPR needs to be combined with defibrillation for best results. -
VF is Always Fatal
With prompt treatment, many people survive VF.
Inspirational Stories of Survival
Stories of those who have overcome VF provide hope and motivation.
-
Athletes Returning to Sports
Some athletes have resumed their careers after surviving VF. -
Everyday Heroes
Ordinary people have saved lives using CPR and AEDs. -
Medical Innovations
Advances in treatment have allowed many to lead normal lives post-VF. -
Community Support
Support groups offer encouragement and shared experiences. -
Personal Resilience
Many survivors find new strength and purpose after their experience.
The Heartbeat of Knowledge
Understanding ventricular fibrillation can be a lifesaver. This chaotic heart rhythm disrupts the heart's ability to pump blood, leading to sudden cardiac arrest. Recognizing symptoms like dizziness, chest pain, or fainting is crucial. Immediate action, such as calling emergency services and performing CPR, can make all the difference.
Defibrillation is the key treatment, using electric shocks to restore a normal heartbeat. Automated External Defibrillators (AEDs) are often found in public places and can be used by anyone. Knowing how to use an AED and perform CPR can save lives.
Prevention involves managing risk factors like heart disease, high blood pressure, and lifestyle choices. Regular check-ups and a healthy lifestyle are essential.
Stay informed, stay prepared, and remember that knowledge is power when it comes to heart health. Your awareness could be the heartbeat that saves a life.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
