Langerhans Cell Histiocytosis (LCH) might sound like a mouthful, but understanding it is crucial for those affected. LCH is a rare disorder where the body produces too many Langerhans cells, a type of white blood cell, leading to tissue damage. These cells, which usually help fight infection, can accumulate in various parts of the body, including bones, skin, and organs. While it primarily affects children, adults aren't immune. Symptoms can vary widely, from skin rashes and bone pain to more severe complications like organ dysfunction. Diagnosing LCH often involves a mix of imaging tests, biopsies, and blood work. Treatment depends on the severity and location of the disease, ranging from observation to chemotherapy. Understanding LCH can help those affected and their families navigate this challenging condition with more confidence and clarity. Let's dive into 50 intriguing facts about LCH to shed light on this complex disorder.
Key Takeaways:
- Langerhans Cell Histiocytosis (LCH) is a rare disorder that affects both children and adults, involving the overproduction of a type of white blood cell called Langerhans cells, which can lead to damage in various tissues and organs.
- LCH is not cancer, but it shares some characteristics with cancer. It can affect multiple systems in the body, and its diagnosis and treatment can be challenging due to its rarity and diverse symptoms.
What is Langerhans Cell Histiocytosis?
Langerhans Cell Histiocytosis (LCH) is a rare disorder that can affect both children and adults. It involves the overproduction of a type of white blood cell called Langerhans cells, which can lead to damage in various tissues and organs.
-
LCH is not cancer. Although it shares some characteristics with cancer, LCH is classified as a histiocytic disorder. It involves the abnormal increase of Langerhans cells, which can form tumors or lesions.
-
Named after Paul Langerhans. The condition is named after the German physician who discovered Langerhans cells in the skin in the 19th century.
-
Affects multiple systems. LCH can impact bones, skin, liver, spleen, lungs, and even the central nervous system, making it a multisystem disorder.
-
Most common in children. While it can occur at any age, LCH is most frequently diagnosed in children between the ages of 1 and 3.
-
Symptoms vary widely. Depending on the organs affected, symptoms can range from skin rashes and bone pain to breathing difficulties and neurological issues.
How is LCH Diagnosed?
Diagnosing LCH can be challenging due to its rarity and the variety of symptoms it presents. Medical professionals use several methods to confirm a diagnosis.
-
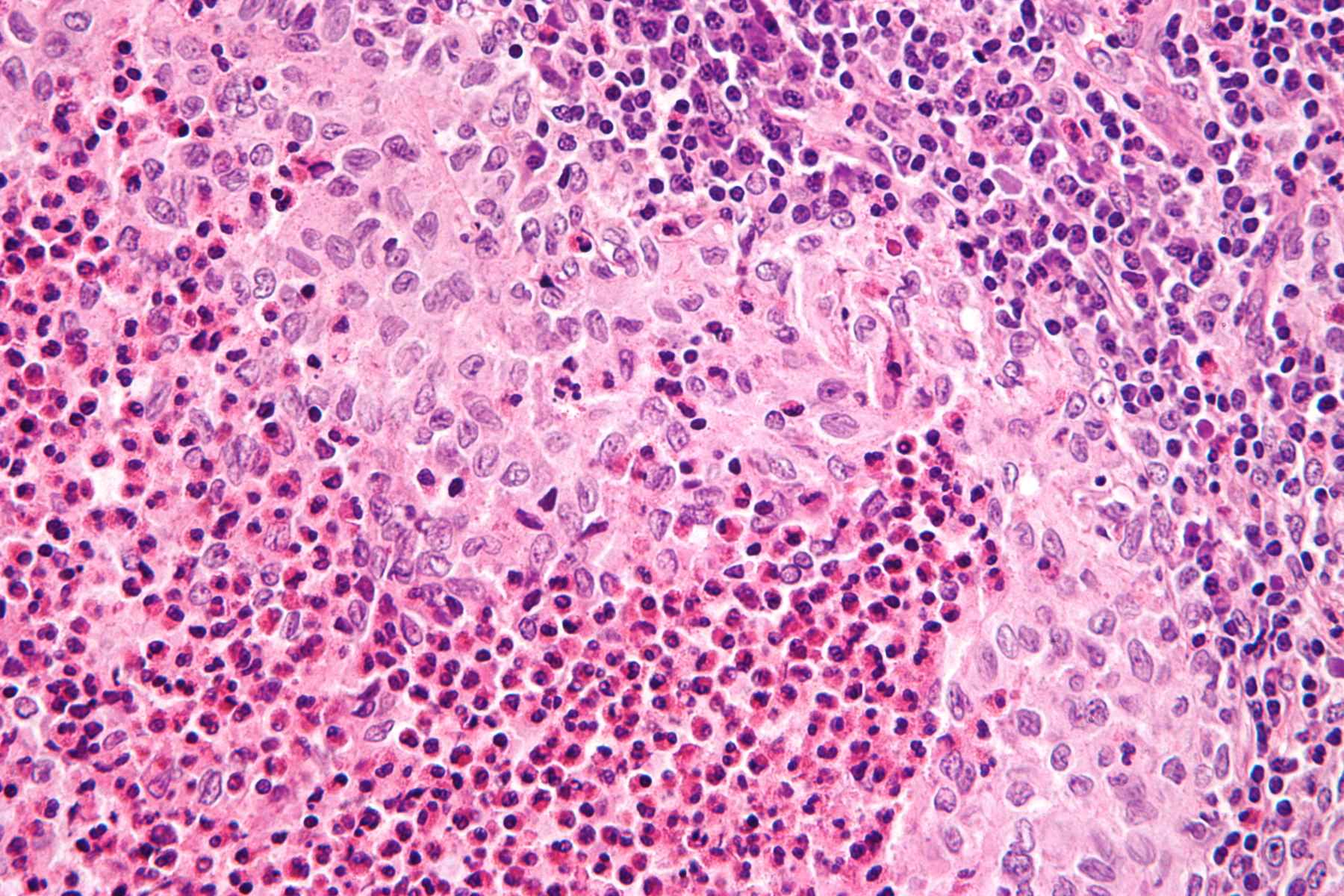
Biopsy is key. A definitive diagnosis often requires a biopsy of the affected tissue to identify the presence of Langerhans cells.
-
Imaging tests help. X-rays, CT scans, and MRIs are commonly used to detect bone lesions or organ involvement.
-
Blood tests are used. While not definitive, blood tests can help assess organ function and rule out other conditions.
-
Bone marrow examination. In some cases, a bone marrow biopsy may be necessary to evaluate the extent of the disease.
-
Differential diagnosis is crucial. LCH symptoms can mimic other diseases, making it important to rule out conditions like infections or other types of cancer.
What Causes LCH?
The exact cause of LCH remains unknown, but researchers have identified several factors that may contribute to its development.
-
Genetic mutations play a role. Mutations in the BRAF gene have been found in a significant number of LCH cases, suggesting a genetic component.
-
Environmental factors are considered. Some studies suggest that environmental exposures, such as tobacco smoke, may increase the risk of developing LCH.
-
Immune system involvement. Abnormal immune responses may trigger the overproduction of Langerhans cells.
-
Not hereditary. Despite the genetic mutations, LCH is not considered a hereditary disease and does not typically run in families.
-
Research is ongoing. Scientists continue to study LCH to better understand its causes and develop more effective treatments.
How is LCH Treated?
Treatment for LCH depends on the severity and location of the disease. Options range from observation to aggressive therapies.
-
Observation for mild cases. In some instances, especially when only the skin is affected, doctors may choose to monitor the condition without immediate treatment.
-
Steroids are commonly used. Corticosteroids can help reduce inflammation and control symptoms in many patients.
-
Chemotherapy for severe cases. More aggressive forms of LCH may require chemotherapy to target and destroy the abnormal cells.
-
Radiation therapy is an option. For localized bone lesions, radiation therapy can be effective in reducing pain and preventing further damage.
-
Surgery is rare. While not common, surgery may be necessary to remove large lesions or tumors that are causing significant problems.
What is the Prognosis for LCH?
The outlook for individuals with LCH varies widely based on several factors, including age, extent of disease, and response to treatment.
-
Prognosis is generally good for children. Many children with LCH respond well to treatment and can lead normal lives.
-
Adults may face more challenges. LCH in adults can be more persistent and may require ongoing management.
-
Risk of recurrence exists. Even after successful treatment, LCH can recur, necessitating regular follow-up care.
-
Long-term effects are possible. Some individuals may experience long-term complications, such as diabetes insipidus or growth problems, especially if the pituitary gland is affected.
-
Support is crucial. Emotional and psychological support for patients and families is an important aspect of managing LCH.
How Common is LCH?
Understanding the prevalence of LCH can help raise awareness and improve diagnosis and treatment strategies.
-
Rare but not unheard of. LCH is considered a rare disease, with an estimated incidence of 1 in 200,000 children.
-
More common in boys. Boys are slightly more likely to develop LCH than girls, though the reasons for this are not fully understood.
-
Global occurrence. LCH affects individuals worldwide, with no specific geographic or ethnic predisposition.
-
Increased awareness. Advances in medical knowledge and technology have improved the ability to diagnose and treat LCH.
-
Support networks exist. Organizations and support groups are available to provide information and assistance to those affected by LCH.
What Research is Being Done on LCH?
Ongoing research aims to uncover more about LCH and improve outcomes for those affected by the disease.
-
Clinical trials are underway. Researchers are conducting clinical trials to test new treatments and therapies for LCH.
-
Genetic studies continue. Scientists are exploring the genetic mutations associated with LCH to develop targeted therapies.
-
Immunotherapy is being explored. New treatments that harness the body's immune system to fight LCH are being investigated.
-
International collaboration. Researchers from around the world are working together to share knowledge and advance understanding of LCH.
-
Patient registries help. Registries that collect data on LCH patients are valuable resources for research and improving patient care.
What Support is Available for LCH Patients?
Support for individuals with LCH and their families is essential for managing the disease and improving quality of life.
-
Patient advocacy groups. Organizations like the Histiocytosis Association provide resources and support for those affected by LCH.
-
Online communities. Social media and online forums offer platforms for patients and families to connect and share experiences.
-
Educational resources. Information about LCH is available through medical centers and advocacy groups to help patients understand their condition.
-
Counseling services. Psychological support can help patients and families cope with the emotional challenges of living with LCH.
-
Financial assistance programs. Some organizations offer financial aid to help cover the costs of treatment and related expenses.
What are the Challenges in LCH Research and Treatment?
Despite advances, there are still challenges in understanding and treating LCH effectively.
-
Rarity complicates research. The rarity of LCH makes it difficult to conduct large-scale studies and gather comprehensive data.
-
Diverse presentation. The wide range of symptoms and organ involvement can complicate diagnosis and treatment decisions.
-
Limited treatment options. While progress has been made, there is still a need for more effective and less toxic treatments.
-
Long-term effects are uncertain. The long-term impact of LCH and its treatments on patients' health and quality of life is not fully understood.
-
Need for awareness. Increasing awareness among healthcare providers and the public is crucial for early diagnosis and intervention.
What are Some Interesting Facts About LCH?
Beyond the medical aspects, there are some intriguing facts about LCH that highlight its complexity and the efforts to combat it.
-
LCH can mimic other diseases. Its symptoms can resemble those of infections, autoimmune disorders, and cancers, making diagnosis challenging.
-
Historical references exist. Cases resembling LCH have been documented in medical literature dating back centuries.
-
Art and LCH. Some artists and writers have used their experiences with LCH as inspiration for their work, raising awareness through creative expression.
-
Celebrity involvement. Public figures have supported LCH research and awareness campaigns, helping to bring attention to the condition.
-
Hope for the future. Advances in genetics and immunology hold promise for more effective treatments and a better understanding of LCH.
Final Thoughts on Langerhans Cell Histiocytosis
Langerhans Cell Histiocytosis (LCH) is a rare disorder that can affect various parts of the body, including skin, bones, and organs. Understanding LCH is crucial for early diagnosis and effective treatment. Though it primarily affects children, adults can also be diagnosed with this condition. Symptoms vary widely, making it tricky to identify without proper medical evaluation. Treatment options range from observation to chemotherapy, depending on the severity and location of the disease. Research is ongoing, offering hope for improved therapies and outcomes. Awareness and education about LCH can lead to better support for those affected and their families. If you suspect any symptoms related to LCH, consulting a healthcare professional is essential. Remember, knowledge is power, and staying informed can make a significant difference in managing health challenges. Stay curious and proactive in learning about rare conditions like LCH.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
