What is a Hydatidiform Mole? A hydatidiform mole, often called a molar pregnancy, is a rare condition where a non-viable fertilized egg implants in the uterus. Instead of developing into a healthy pregnancy, it turns into an abnormal growth. This growth resembles a cluster of grapes and is caused by a problem during fertilization. There are two types: complete and partial. Complete moles have no normal fetal tissue, while partial moles may have some but are still not viable. Though not cancerous, they can lead to complications if not treated. Symptoms might include unusual bleeding, severe nausea, or rapid uterine growth. Diagnosing involves ultrasound and blood tests. Treatment usually requires surgical removal. It's crucial to monitor hormone levels afterward to ensure no tissue remains. Understanding this condition helps in managing it effectively and ensuring future pregnancies are healthy.
Key Takeaways:
- Hydatidiform mole is a rare condition affecting pregnancies, with symptoms mimicking normal pregnancy. Early detection and regular follow-up are crucial for effective management and recovery.
- Understanding the causes, risk factors, and symptoms of hydatidiform mole can help in early diagnosis and effective treatment. Regular monitoring and emotional support are essential for recovery and future pregnancies.
Understanding Hydatidiform Mole
Hydatidiform mole, often called a molar pregnancy, is a rare condition that affects pregnancies. It involves abnormal growth of trophoblasts, the cells that normally develop into the placenta. Here are some intriguing facts about this condition.
-
Rare Occurrence: Hydatidiform mole occurs in about 1 in every 1,000 pregnancies. This rarity makes it a unique condition in obstetrics.
-
Two Types: There are two main types: complete and partial. Complete moles have no normal fetal tissue, while partial moles may have some normal tissue but are still abnormal.
-
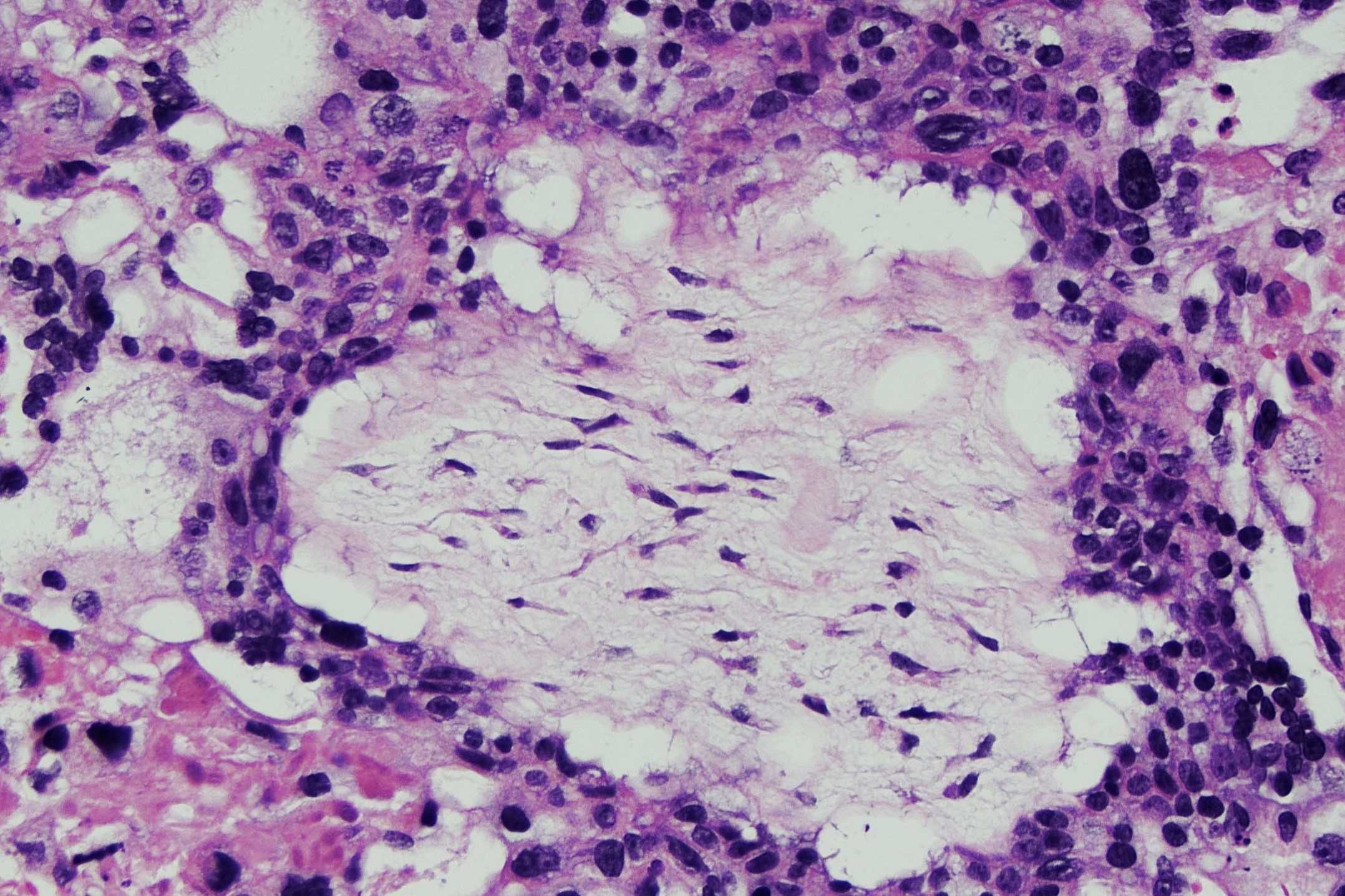
Grape-like Appearance: The name "hydatidiform" comes from the Greek word for "water drop," reflecting the grape-like clusters of cysts that form.
-
Chromosomal Abnormalities: Complete moles usually have 46 chromosomes, all from the father, while partial moles have 69 chromosomes, with an extra set from the father.
-
Symptoms Mimic Pregnancy: Symptoms can include severe nausea, vomiting, and rapid uterine growth, often mistaken for a normal pregnancy.
-
High hCG Levels: Women with this condition often have higher than normal levels of human chorionic gonadotropin (hCG), a hormone produced during pregnancy.
-
Ultrasound Diagnosis: An ultrasound can reveal the characteristic "snowstorm" pattern, indicating a molar pregnancy.
-
Risk Factors: Women under 20 or over 35, and those with a history of molar pregnancy, are at higher risk.
-
Treatment Involves Removal: Treatment typically involves surgical removal of the mole through a procedure called dilation and curettage (D&C).
-
Follow-Up Care: Regular follow-up is crucial to monitor hCG levels and ensure no remaining molar tissue.
Causes and Risk Factors
Understanding what causes a hydatidiform mole and who is at risk can help in early detection and management.
-
Genetic Factors: Abnormal fertilization is the primary cause, often involving two sperm fertilizing one egg.
-
Nutritional Deficiencies: Some studies suggest a link between low carotene or vitamin A intake and increased risk.
-
Previous Molar Pregnancy: Women who have had one molar pregnancy have a higher chance of experiencing another.
-
Geographic Variations: Incidence rates vary worldwide, with higher occurrences in Southeast Asia and Latin America.
-
Blood Type Influence: Some research indicates women with blood type A or AB may have a slightly higher risk.
-
Family History: Rarely, a family history of molar pregnancies can increase risk, suggesting a genetic component.
-
Age Factor: Women over 40 have a significantly higher risk compared to younger women.
-
Reproductive History: Women with a history of miscarriage or infertility may face increased risk.
-
Environmental Factors: Exposure to certain environmental toxins may contribute, though evidence is limited.
-
Hormonal Imbalances: Imbalances in reproductive hormones might play a role in the development of molar pregnancies.
Symptoms and Diagnosis
Recognizing symptoms and understanding diagnostic methods are key to managing hydatidiform mole effectively.
-
Vaginal Bleeding: One of the most common symptoms is abnormal vaginal bleeding during early pregnancy.
-
Pelvic Pain: Some women experience pelvic pain or pressure due to the rapid growth of the uterus.
-
Hyperemesis Gravidarum: Severe nausea and vomiting, known as hyperemesis gravidarum, can be a sign.
-
Preeclampsia: Early-onset preeclampsia, a condition characterized by high blood pressure, may occur.
-
Thyroid Issues: Elevated hCG levels can mimic thyroid-stimulating hormone, leading to hyperthyroidism symptoms.
-
Ultrasound Imaging: Ultrasound is the primary tool for diagnosing molar pregnancies, revealing characteristic patterns.
-
Blood Tests: Blood tests measuring hCG levels help confirm the diagnosis and monitor treatment progress.
-
Tissue Analysis: After removal, the tissue is analyzed to confirm the diagnosis and type of mole.
-
Chest X-ray: In some cases, a chest X-ray is done to check for metastasis, though rare in hydatidiform mole.
-
MRI or CT Scan: These imaging techniques may be used if there is suspicion of complications or spread.
Treatment and Management
Effective treatment and management strategies are crucial for recovery and future pregnancies.
-
Surgical Removal: Dilation and curettage (D&C) is the standard procedure to remove molar tissue.
-
Hysterectomy Option: In some cases, especially for women who do not wish to have more children, a hysterectomy may be considered.
-
Chemotherapy: If the mole becomes cancerous, chemotherapy may be necessary to treat gestational trophoblastic neoplasia.
-
hCG Monitoring: Regular monitoring of hCG levels post-treatment ensures no remaining molar tissue.
-
Contraception Advice: Women are advised to avoid pregnancy for at least six months to a year after treatment.
-
Emotional Support: Psychological support and counseling can help women cope with the emotional impact.
-
Nutritional Support: Ensuring adequate nutrition, particularly vitamin A, may aid recovery.
-
Regular Follow-Ups: Frequent medical check-ups are essential to monitor recovery and prevent complications.
-
Fertility Considerations: Most women can have normal pregnancies after treatment, though they may need closer monitoring.
-
Support Groups: Joining support groups can provide emotional and practical support from others with similar experiences.
Complications and Prognosis
While most cases resolve with treatment, understanding potential complications and prognosis is important.
-
Persistent GTD: In some cases, molar tissue can persist, leading to gestational trophoblastic disease (GTD).
-
Choriocarcinoma Risk: Rarely, a molar pregnancy can develop into choriocarcinoma, a malignant form of GTD.
-
Metastasis: Though uncommon, molar tissue can spread to other parts of the body, requiring more intensive treatment.
-
Recurrence Risk: Women who have had a molar pregnancy have a slightly increased risk of recurrence in future pregnancies.
-
Fertility Impact: Most women retain normal fertility after treatment, though some may experience complications.
-
Emotional Impact: The emotional toll of a molar pregnancy can be significant, requiring psychological support.
-
Long-term Monitoring: Continued monitoring of hCG levels is crucial to detect any recurrence or complications.
-
Survival Rates: With proper treatment, the prognosis is excellent, with high survival rates even in cases of malignant transformation.
-
Future Pregnancies: Women can typically have healthy pregnancies after a molar pregnancy, though they may need closer monitoring.
-
Research Advances: Ongoing research aims to better understand the causes and improve treatment options for hydatidiform mole.
Final Thoughts on Hydatidiform Mole
Hydatidiform mole, a rare pregnancy complication, can be a bit of a mystery. It's crucial to understand that this condition involves abnormal growth of trophoblastic tissue in the uterus. While it might sound scary, early detection and treatment often lead to positive outcomes. Regular prenatal care plays a big role in catching any signs early. Symptoms like vaginal bleeding, severe nausea, or rapid uterine growth shouldn't be ignored. If diagnosed, treatment usually involves a procedure called dilation and curettage to remove the mole. Follow-up care is important to ensure no further complications. Though it can be a challenging experience, support from healthcare providers and loved ones makes a big difference. Remember, knowledge is power. Understanding the facts about hydatidiform mole helps in managing it effectively and reduces anxiety. Stay informed and proactive about your health.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
