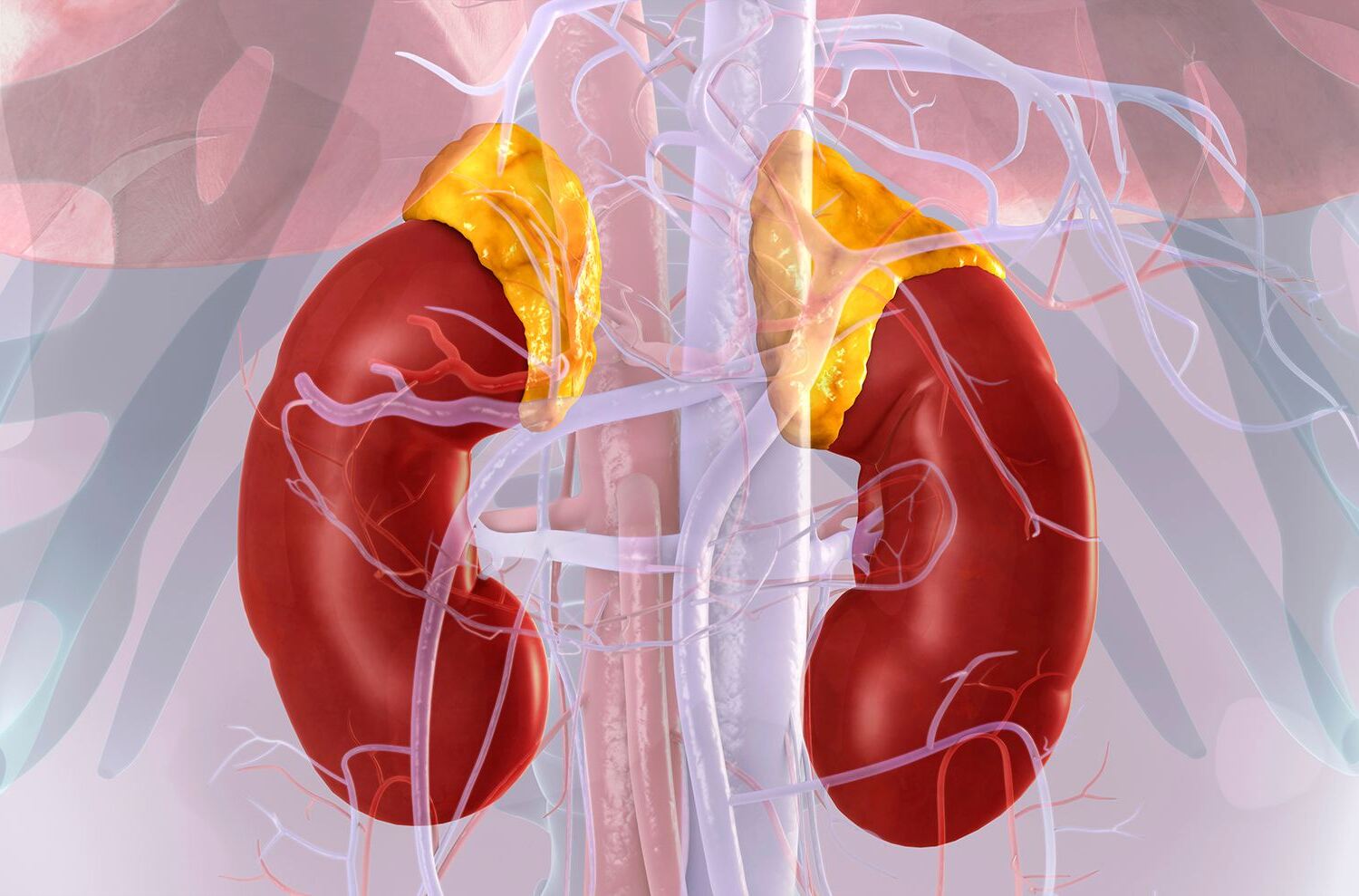
What is Addison's Disease? Addison's disease, also known as primary adrenal insufficiency, is a rare disorder where the adrenal glands fail to produce enough cortisol and aldosterone. Affecting roughly 1 in 100,000 people in the United States, it can strike anyone but is most common between ages 30 and 50, with women being more frequently affected. Symptoms often sneak up slowly, causing fatigue, muscle weakness, weight loss, and darkened skin patches. If untreated, it can lead to a life-threatening adrenal crisis. Understanding Addison's disease is crucial for early diagnosis and effective management, ensuring those affected can lead healthy lives.
Key Takeaways:
- Addison's Disease is a rare condition where the adrenal glands don't produce enough essential hormones, leading to symptoms like fatigue, skin changes, and increased thirst. Early diagnosis and proper management are crucial.
- Patients with Addison's Disease need lifelong hormone replacement therapy and regular monitoring to prevent complications. Family support, workplace accommodations, and emergency preparedness are essential for effective management and quality of life.
What is Addison's Disease?
Addison's disease, also known as primary adrenal insufficiency, is a rare condition where the adrenal glands don't produce enough essential hormones. This can lead to a variety of symptoms and complications if not managed properly.
- Definition: Addison's disease is a rare disorder where the adrenal glands do not produce enough cortisol and aldosterone, leading to a range of symptoms.
- Prevalence: It affects approximately 1 in 100,000 people in the United States, making it a rare condition.
- Age Range: The condition can affect people of all ages, but it is most common between the ages of 30 and 50.
- Gender Distribution: Addison's disease is more common in women than men.
Causes and Risk Factors
Understanding the causes and risk factors can help in early diagnosis and management of Addison's disease.
- Causes: The most common cause of Addison's disease is an autoimmune response, where the immune system mistakenly attacks the adrenal glands.
- Autoimmune Response: Approximately 75% of cases are due to an autoimmune attack, which can occur as an isolated condition or as part of autoimmune polyendocrine syndromes (APS type-1 and II).
- Other Causes: Less common causes include tuberculosis, infections such as fungal infections, cancer, bleeding into the adrenal gland, and amyloidosis.
- Risk Factors: Risk factors for autoimmune Addison's disease include other autoimmune conditions such as type I diabetes, hypoparathyroidism, hypopituitarism, pernicious anemia, Graves' disease, chronic thyroiditis, dermatitis herpetiformis, vitiligo, and myasthenia gravis.
Symptoms of Addison's Disease
Symptoms can vary widely and often develop slowly, making early diagnosis challenging.
- Symptoms: Symptoms of Addison's disease typically develop slowly and can include fatigue, muscle weakness, low mood, loss of appetite, and unintentional weight loss.
- Skin Changes: One of the distinctive symptoms is hyperpigmentation, which can cause darkened skin patches, particularly in areas like the knuckles and gums.
- Vitiligo: Some individuals may also develop vitiligo, characterized by white patches on the skin.
- Dark Freckles: Black freckles may appear on the forehead, face, or shoulders in some cases.
- Mucous Membrane Discoloration: Dark blue spots can appear inside the mouth, rectum, or vagina.
- Fatigue: Fatigue is the most common initial symptom of Addison's disease.
- Muscle Weakness: Muscle weakness is another common symptom that can lead to difficulty standing or walking.
- Low Mood: Low mood or depression can also be a symptom, which may be mistaken for clinical depression.
- Loss of Appetite: Loss of appetite and subsequent weight loss are common due to the body's inability to regulate blood sugar levels properly.
- Increased Thirst: Increased thirst and urination can occur due to the imbalance of sodium and potassium levels in the blood.
Adrenal Crisis
An adrenal crisis is a severe complication that requires immediate medical attention.
- Adrenal Crisis: An adrenal crisis is a life-threatening emergency that can occur when the levels of cortisol in the body fall significantly. Symptoms include severe belly pain, muscle weakness, and dangerously low blood pressure.
- Emergency Treatment: In the event of an adrenal crisis, immediate treatment involves administering hydrocortisone injections and IV fluids to stabilize blood pressure and prevent further complications.
Diagnosis and Testing
Proper diagnosis is crucial for effective treatment and management of Addison's disease.
- Diagnosis: Diagnosis is often delayed due to the nonspecific nature of the symptoms, which can resemble those of more common conditions like clinical depression or flu.
- Blood Tests: Blood tests are crucial for diagnosing Addison's disease, measuring sodium and potassium levels, and adrenal and pituitary hormone levels.
- Pituitary Hormone Test: Sometimes, doctors inject pituitary hormones to see if the adrenal glands can respond to them, which helps in diagnosing secondary adrenal insufficiency.
- Clinical Suspicion: Maintaining a high clinical suspicion is crucial to avoid misdiagnosis. Early recognition is essential to prevent severe complications.
Treatment and Management
Treatment focuses on hormone replacement and managing symptoms to ensure a good quality of life.
- Treatment: The primary treatment for Addison's disease involves replacing the missing hormones with medication. Patients need to take these hormones for the rest of their lives.
- Medication: The medication typically prescribed includes hydrocortisone and fludrocortisone to replace cortisol and aldosterone, respectively.
- Management: Management involves lifelong hormone replacement therapy and awareness of the risk of adrenal crises. Patients need to carry a card or bracelet indicating their condition and medication list.
- Lifestyle Adjustments: Patients with Addison's disease often need to make lifestyle adjustments to manage fatigue and associated health conditions like diabetes or hypothyroidism.
- Monitoring: Regular monitoring of hormone levels and blood pressure is essential to ensure that the condition is well-managed and to prevent complications.
Complications and Associated Conditions
Addison's disease can lead to various complications if not properly managed.
- Infections: Infectious causes include sepsis, tuberculosis, cytomegalovirus, HIV, disseminated fungal infections like histoplasmosis, and syphilis.
- Adrenal Hemorrhage: Adrenal hemorrhage can be caused by conditions like DIC (disseminated intravascular coagulation), trauma, meningococcemia, and neoplastic processes. The Waterhouse-Friderichsen syndrome is a specific type of adrenal crisis due to meningococcemia.
- Blastomycosis: Blastomycosis is another cause of Addison disease, particularly in South America.
- Amyloidosis: Amyloidosis is a condition where abnormal proteins accumulate in the adrenal glands, leading to their dysfunction.
- Tuberculosis: Historically, tuberculosis was a major cause of Addison's disease but remains a significant cause in developing countries.
Living with Addison's Disease
Living with Addison's disease requires ongoing management and support.
- Delayed Diagnosis: The nonspecific nature of the symptoms often leads to delays in proper diagnosis. Healthcare providers may accidentally discover Addison's disease during routine blood tests showing low sodium or high potassium levels.
- Acute Adrenal Crisis: An acute adrenal crisis is a medical emergency characterized by hypotension, hyponatremia, hyperkalemia, and hypoglycemia. Immediate treatment with hydrocortisone injections and IV fluids is necessary.
- Emergency Preparedness: Patients need to be prepared for emergencies by carrying emergency medication and knowing how to administer it correctly. They should also have a plan in place for how to handle an adrenal crisis.
- Family Support: Family support is essential for managing the condition effectively. Educating family members about the condition and its management can help them provide better care.
- Workplace Accommodations: Patients may need to make workplace accommodations to manage their condition effectively. This can include flexible working hours or regular breaks to rest.
- Travel Precautions: Travel precautions are necessary to ensure that patients have access to medical care in case of an emergency. Carrying a medical alert card or bracelet can help in such situations.
Research and Awareness
Ongoing research and public awareness are vital for improving the lives of those with Addison's disease.
- Research: Ongoing research aims to better understand the causes of Addison's disease and to develop more effective treatments. The National Congenital Anomaly and Rare Disease Registration Service (NCARDRS) helps scientists look for better ways to prevent and treat this condition.
- Public Awareness: Raising public awareness about Addison's disease is crucial to ensure early diagnosis and proper management. Many organizations provide resources and support for patients and their families.
- Support Groups: Joining support groups can provide emotional support and help patients cope with the condition more effectively.
- Psychological Impact: The chronic nature of the condition can have a significant psychological impact on patients, including anxiety and depression. Mental health support is often necessary.
- Quality of Life: With proper management, most people with Addison's disease can lead a normal life with few limitations. However, managing bouts of fatigue and associated health conditions is crucial for maintaining a good quality of life.
Genetic and Environmental Factors
Both genetic and environmental factors can play a role in the development of Addison's disease.
- Genetic Factors: While not the primary cause, genetic factors can play a role in the development of autoimmune Addison's disease, particularly in the context of autoimmune polyendocrine syndromes.
- Environmental Factors: The exact environmental triggers for autoimmune Addison's disease are not well-understood but may include viral infections or other environmental stressors.
Monitoring and Regular Check-ups
Regular check-ups and monitoring are essential for managing Addison's disease effectively.
- Monitoring: Regular monitoring of hormone levels and blood pressure is essential to ensure that the condition is well-managed and to prevent complications.
- Clinical Suspicion: Maintaining a high clinical suspicion is crucial to avoid misdiagnosis. Early recognition is essential to prevent severe complications.
- Lifestyle Adjustments: Patients with Addison's disease often need to make lifestyle adjustments to manage fatigue and associated health conditions like diabetes or hypothyroidism.
Living with Addison's Disease
Living with Addison's disease means constant vigilance and lifelong hormone replacement therapy. Symptoms like fatigue, muscle weakness, and skin changes can significantly impact daily life. Recognizing the signs early is crucial for timely diagnosis and treatment. Regular monitoring of hormone levels and blood pressure helps manage the condition effectively.
Patients need to be prepared for emergencies, carrying a medical alert card or bracelet and knowing how to administer emergency medication. Support from family, friends, and support groups can make a big difference in coping with the psychological impact.
Despite the challenges, with proper management, most people with Addison's disease can lead a normal life. Awareness and education about this rare condition are key to improving the quality of life for those affected. Stay informed, stay prepared, and live life to the fullest.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
