Islet cell carcinoma, also known as pancreatic neuroendocrine tumor (PNET), is a rare type of cancer that forms in the hormone-producing cells of the pancreas. Islet cell carcinoma is different from the more common pancreatic adenocarcinoma. Understanding this cancer can be challenging due to its rarity and the complexity of its symptoms. These tumors can be functional, producing hormones that cause noticeable symptoms, or non-functional, often going unnoticed until they grow large. Common symptoms include abdominal pain, weight loss, and jaundice. Treatment options vary, including surgery, chemotherapy, and targeted therapies, depending on the tumor's size and spread. Early detection is crucial for better outcomes, but this can be difficult due to vague symptoms. Learning about islet cell carcinoma helps in recognizing its signs and understanding treatment possibilities. With ongoing research, hope remains for improved therapies and outcomes for those affected by this uncommon disease.
Key Takeaways:
- Islet cell carcinoma, a rare pancreatic cancer, can cause varied symptoms and requires specialized diagnosis and treatment. Early detection and ongoing research offer hope for improved outcomes.
- Patients with islet cell carcinoma can benefit from a range of treatment options, support resources, and lifestyle adjustments to manage the condition and maintain a good quality of life.
Understanding Islet Cell Carcinoma
Islet cell carcinoma, also known as pancreatic neuroendocrine tumors (PNETs), is a rare type of cancer that begins in the hormone-producing cells of the pancreas. These tumors can be either benign or malignant, and they often present unique challenges in diagnosis and treatment. Let's explore some intriguing facts about this uncommon condition.
-
Rare Occurrence
Islet cell carcinoma accounts for only about 1-2% of all pancreatic cancers. This rarity makes it a unique focus for medical research and treatment strategies. -
Hormone Production
These tumors originate from islet cells, which are responsible for producing hormones like insulin and glucagon. This can lead to various symptoms depending on the hormones affected. -
Functional vs. Non-functional
Islet cell tumors are classified as functional or non-functional. Functional tumors produce excess hormones, causing noticeable symptoms, while non-functional ones may not produce hormones or symptoms until they grow large. -
Multiple Endocrine Neoplasia Type 1 (MEN1)
A genetic condition called MEN1 increases the risk of developing islet cell carcinoma. Individuals with MEN1 often have tumors in multiple endocrine glands. -
Slow Growth
Compared to other pancreatic cancers, islet cell carcinomas generally grow more slowly. This can sometimes lead to a better prognosis if detected early.
Symptoms and Diagnosis
Recognizing the symptoms of islet cell carcinoma can be challenging due to their variability. Diagnosis often requires a combination of tests and imaging techniques.
-
Varied Symptoms
Symptoms can range from abdominal pain and weight loss to more specific signs like hypoglycemia or skin rashes, depending on the hormones involved. -
Imaging Techniques
CT scans, MRIs, and PET scans are commonly used to detect and evaluate these tumors. These imaging methods help determine the tumor's size and spread. -
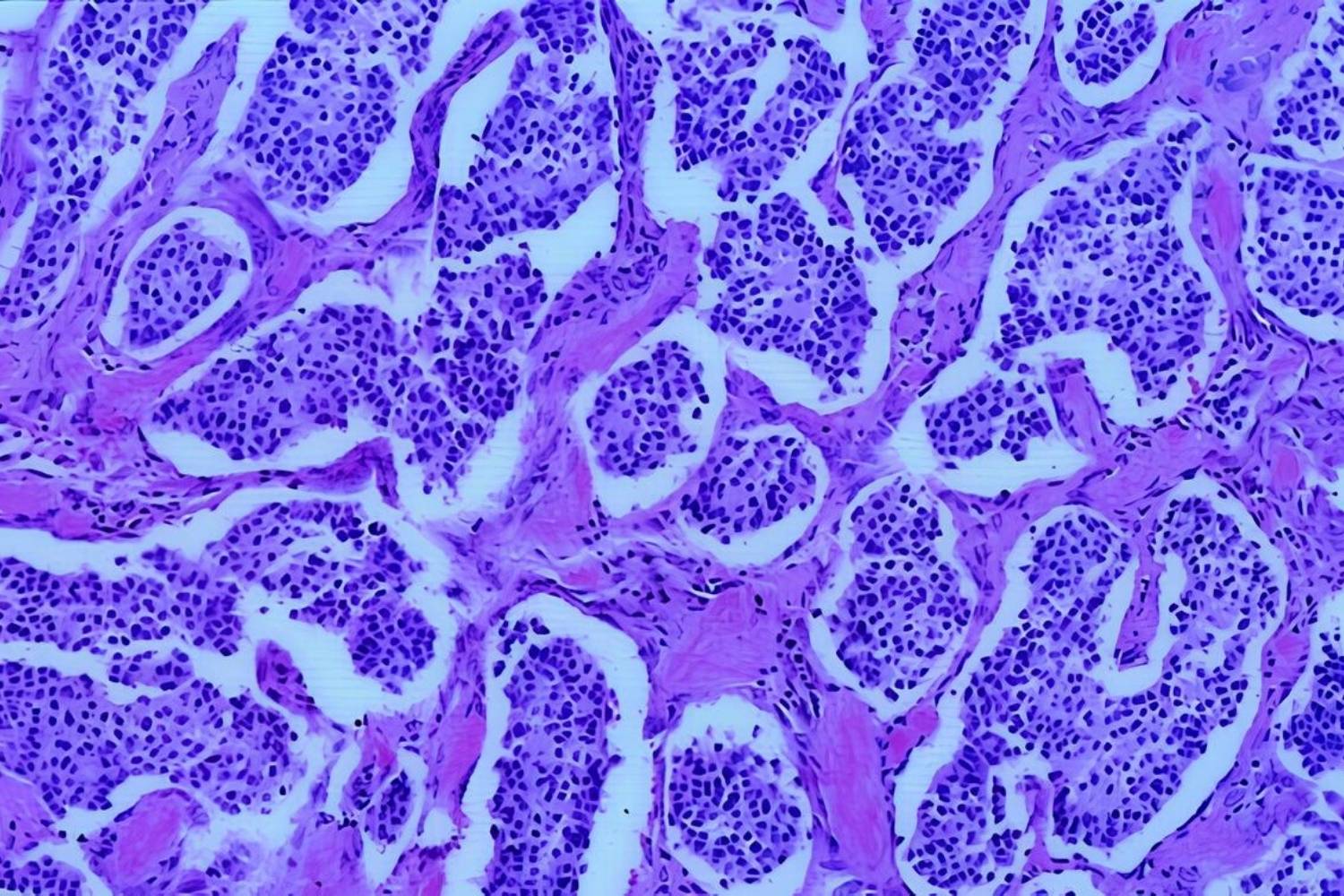
Biopsy for Confirmation
A biopsy is often necessary to confirm the diagnosis. This involves taking a small tissue sample from the tumor for microscopic examination. -
Blood Tests
Blood tests measuring hormone levels can aid in diagnosing functional islet cell tumors. Elevated hormone levels can indicate the presence of a tumor. -
Genetic Testing
For those with a family history of MEN1 or other genetic conditions, genetic testing can help assess the risk of developing islet cell carcinoma.
Treatment Options
Treatment for islet cell carcinoma varies based on the tumor's size, location, and whether it has spread. Here are some common approaches.
-
Surgical Removal
Surgery is often the primary treatment for localized tumors. Removing the tumor can alleviate symptoms and prevent further spread. -
Chemotherapy
Chemotherapy may be used for advanced cases or when surgery isn't possible. It helps shrink tumors and slow their growth. -
Targeted Therapy
Targeted therapies focus on specific molecules involved in tumor growth. These treatments can be effective with fewer side effects than traditional chemotherapy. -
Hormone Therapy
For functional tumors, hormone therapy can help manage symptoms by controlling hormone production. -
Radiation Therapy
Radiation may be used to target and destroy cancer cells, especially if the tumor has spread to other parts of the body.
Prognosis and Research
The prognosis for islet cell carcinoma varies widely, but ongoing research continues to improve understanding and treatment.
-
Variable Prognosis
Prognosis depends on factors like tumor size, location, and whether it has metastasized. Early detection often leads to better outcomes. -
Survival Rates
The five-year survival rate for localized islet cell carcinoma can be as high as 60-80%, but it decreases significantly if the cancer has spread. -
Research Advances
Ongoing research aims to develop new treatments and improve early detection methods. Clinical trials are exploring innovative therapies. -
Immunotherapy Potential
Immunotherapy, which harnesses the body's immune system to fight cancer, is being studied as a potential treatment for islet cell carcinoma. -
Patient Support
Support groups and counseling can be valuable resources for patients and families dealing with islet cell carcinoma, providing emotional and practical assistance.
Living with Islet Cell Carcinoma
Living with islet cell carcinoma involves managing symptoms and maintaining a good quality of life. Here are some aspects to consider.
-
Regular Monitoring
Regular follow-up appointments and monitoring are crucial for managing the condition and detecting any changes early. -
Dietary Adjustments
Dietary changes may be necessary, especially for those with functional tumors affecting insulin production. A nutritionist can help tailor a suitable diet plan. -
Pain Management
Pain management strategies, including medications and therapies, can help alleviate discomfort associated with the condition. -
Emotional Well-being
Coping with a cancer diagnosis can be challenging. Mental health support, including therapy and support groups, can be beneficial. -
Family Involvement
Involving family members in the care process can provide additional support and help manage the practical aspects of living with the condition.
Prevention and Awareness
While there are no guaranteed ways to prevent islet cell carcinoma, awareness and early detection can make a significant difference.
-
Regular Check-ups
Regular medical check-ups can help detect any unusual symptoms early, especially for those with a family history of related conditions. -
Healthy Lifestyle
Maintaining a healthy lifestyle, including a balanced diet and regular exercise, can contribute to overall well-being and potentially reduce cancer risk. -
Avoiding Risk Factors
Avoiding known risk factors, such as smoking and excessive alcohol consumption, can help lower the risk of developing various types of cancer. -
Genetic Counseling
For those with a family history of MEN1 or other genetic conditions, genetic counseling can provide valuable information and guidance. -
Public Awareness
Raising public awareness about islet cell carcinoma can lead to earlier detection and improved outcomes for those affected.
Future Directions in Research
Research into islet cell carcinoma is ongoing, with scientists exploring new avenues for treatment and understanding.
-
Genomic Studies
Genomic studies are helping identify genetic mutations associated with islet cell carcinoma, paving the way for personalized treatments. -
Biomarker Discovery
Researchers are working to discover biomarkers that can aid in early detection and monitoring of the disease. -
Combination Therapies
Combining different treatment modalities, such as chemotherapy and targeted therapy, is being investigated to improve outcomes. -
Patient Registries
Patient registries collect data on individuals with islet cell carcinoma, providing valuable insights for research and treatment development. -
International Collaboration
International collaboration among researchers and medical institutions is advancing the understanding and treatment of this rare cancer.
Support and Resources
Support and resources are essential for patients and families navigating the challenges of islet cell carcinoma.
-
Patient Advocacy Groups
Patient advocacy groups offer support, information, and resources for those affected by islet cell carcinoma. -
Online Communities
Online communities provide a platform for patients and families to connect, share experiences, and offer support. -
Educational Materials
Educational materials, including brochures and online resources, can help patients and families better understand the condition and treatment options. -
Financial Assistance
Financial assistance programs may be available to help cover the costs of treatment and related expenses. -
Healthcare Team
A dedicated healthcare team, including oncologists, surgeons, and support staff, plays a crucial role in managing islet cell carcinoma and providing comprehensive care.
Final Thoughts on Islet Cell Carcinoma
Islet cell carcinoma, also known as pancreatic neuroendocrine tumors, is a rare but significant type of cancer. Understanding its symptoms, diagnosis, and treatment options is crucial for managing this condition. Early detection can make a big difference in outcomes, so being aware of signs like abdominal pain, weight loss, and changes in blood sugar levels is important. Treatments range from surgery to targeted therapies, offering hope for those affected. Research continues to advance, bringing new insights and potential therapies. Support from healthcare professionals, family, and friends plays a vital role in navigating this journey. Staying informed and proactive can empower patients and their loved ones to make the best decisions for their health. Remember, knowledge is power, and staying educated about islet cell carcinoma can lead to better management and improved quality of life.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
