Hereditary Non-Spherocytic Hemolytic Anemia (HNSHA) is a rare blood disorder. It affects the red blood cells, causing them to break down faster than normal. This condition is inherited, meaning it passes from parents to children through genes. People with HNSHA often experience fatigue, jaundice, and an enlarged spleen. HNSHA can be tricky to diagnose because its symptoms overlap with other types of anemia. Treatment usually focuses on managing symptoms and may include blood transfusions or medications. Understanding the basics of HNSHA can help those affected and their families navigate this challenging condition. Let's dive into 40 facts about Hereditary Non-Spherocytic Hemolytic Anemia to shed light on its causes, symptoms, and treatments.
Key Takeaways:
- Hereditary Non-Spherocytic Hemolytic Anemia (HNSHA) is a rare genetic disorder that affects red blood cells, causing anemia and other symptoms. It can be inherited from both parents and has various treatment options.
- People with HNSHA may experience symptoms like fatigue, jaundice, and an enlarged spleen. Treatment options include folic acid supplements, blood transfusions, and genetic testing for diagnosis. Ongoing research aims to develop new treatments.
What is Hereditary Non-Spherocytic Hemolytic Anemia?
Hereditary Non-Spherocytic Hemolytic Anemia (HNSHA) is a rare genetic disorder affecting red blood cells. It causes these cells to break down prematurely, leading to anemia. Let's dive into some fascinating facts about this condition.
-
HNSHA is inherited in an autosomal recessive manner. This means both parents must carry the gene for a child to be affected.
-
The disorder affects the red blood cells' ability to maintain their shape. Unlike spherocytic anemia, the cells do not become spherical but still break down easily.
-
HNSHA can be caused by mutations in various genes. These include G6PD, PKLR, and others that are crucial for red blood cell metabolism.
-
Symptoms often appear in infancy or early childhood. These can include fatigue, jaundice, and an enlarged spleen.
-
The severity of symptoms can vary widely. Some individuals may have mild anemia, while others experience severe complications.
Symptoms and Diagnosis
Understanding the symptoms and how HNSHA is diagnosed can help in managing the condition effectively.
-
Common symptoms include pale skin, shortness of breath, and rapid heartbeat. These are typical signs of anemia.
-
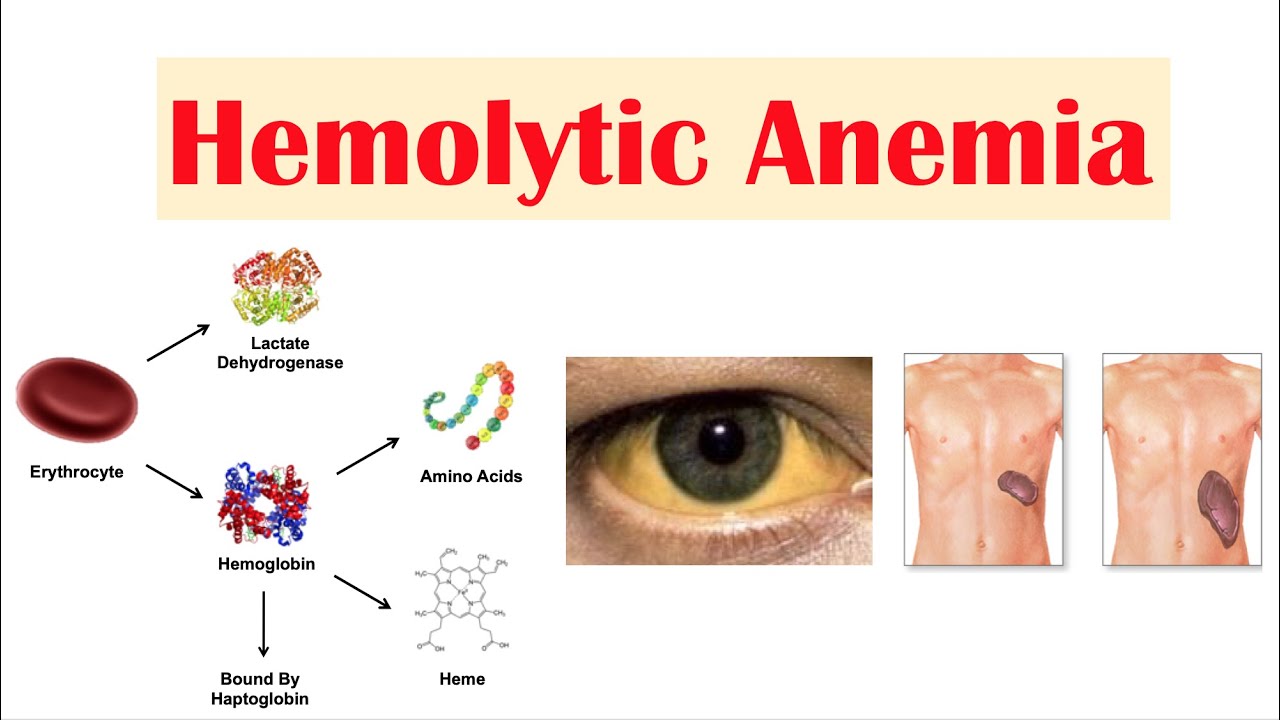
Jaundice is a frequent symptom. This yellowing of the skin and eyes occurs due to the breakdown of red blood cells.
-
An enlarged spleen is often observed. The spleen works harder to remove the defective red blood cells, causing it to swell.
-
Diagnosis typically involves blood tests. These tests measure hemoglobin levels and look for abnormal red blood cells.
-
Genetic testing can confirm the diagnosis. Identifying the specific gene mutation helps in understanding the condition better.
Treatment Options
While there is no cure for HNSHA, various treatments can help manage the symptoms and improve quality of life.
-
Folic acid supplements are commonly prescribed. They help in the production of new red blood cells.
-
Blood transfusions may be necessary in severe cases. This helps to maintain adequate hemoglobin levels.
-
Splenectomy, or removal of the spleen, can be considered. This procedure reduces the destruction of red blood cells.
-
Iron chelation therapy may be needed. Frequent blood transfusions can lead to iron overload, which this therapy helps to manage.
-
Regular monitoring is crucial. Frequent check-ups help in managing the condition and adjusting treatments as needed.
Genetic Aspects
The genetic basis of HNSHA is complex, involving multiple genes and inheritance patterns.
-
Mutations in the G6PD gene are a common cause. This gene is crucial for protecting red blood cells from damage.
-
The PKLR gene is another significant player. Mutations here affect the enzyme pyruvate kinase, essential for red blood cell energy production.
-
Other genes like SLC4A1 and ALDOA can also be involved. Each gene mutation affects red blood cells differently.
-
Carrier parents have a 25% chance of having an affected child. This is typical for autosomal recessive disorders.
-
Genetic counseling is recommended for affected families. It helps in understanding the risks and implications of the disorder.
Living with HNSHA
Managing daily life with HNSHA involves various strategies to cope with symptoms and maintain health.
-
A balanced diet rich in vitamins and minerals is essential. This supports overall health and red blood cell production.
-
Avoiding certain medications is crucial. Some drugs can trigger hemolysis in individuals with HNSHA.
-
Regular exercise can help. It improves overall fitness and energy levels, though it should be tailored to the individual's capacity.
-
Staying hydrated is important. Proper hydration supports red blood cell function and overall health.
-
Joining support groups can be beneficial. Connecting with others who have HNSHA provides emotional support and practical advice.
Research and Future Directions
Ongoing research aims to better understand HNSHA and develop new treatments.
-
Gene therapy holds promise. Researchers are exploring ways to correct the genetic mutations causing HNSHA.
-
New medications are being tested. These aim to improve red blood cell stability and reduce hemolysis.
-
Clinical trials are ongoing. Participation in trials can provide access to cutting-edge treatments.
-
Research into the molecular mechanisms continues. Understanding how gene mutations affect red blood cells helps in developing targeted therapies.
-
Patient registries are being established. These databases collect information to improve understanding and management of HNSHA.
Interesting Facts
Here are some lesser-known but intriguing facts about HNSHA.
-
HNSHA is more common in certain populations. For example, G6PD deficiency is prevalent in people of African, Mediterranean, and Asian descent.
-
The disorder can be triggered by infections. Certain illnesses can exacerbate hemolysis in affected individuals.
-
Some foods can trigger symptoms. Fava beans, for instance, can cause hemolysis in people with G6PD deficiency.
-
HNSHA can sometimes be mistaken for other types of anemia. Accurate diagnosis is crucial for proper management.
-
The condition can affect both males and females. Unlike some genetic disorders, HNSHA does not have a gender preference.
Support and Resources
Various resources are available to help those affected by HNSHA.
-
Patient advocacy groups provide support. Organizations like the National Organization for Rare Disorders offer resources and information.
-
Online forums and communities can be helpful. These platforms allow individuals to share experiences and advice.
-
Educational materials are available. Books, articles, and videos can help in understanding and managing HNSHA.
-
Healthcare providers play a key role. Regular consultations with doctors and specialists are essential.
-
Financial assistance programs exist. These can help cover the costs of treatments and medications.
Final Thoughts on Hereditary Non-Spherocytic Hemolytic Anemia
Hereditary Non-Spherocytic Hemolytic Anemia (HNSHA) is a complex condition that affects red blood cells, leading to their premature destruction. Understanding its genetic basis, symptoms, and treatment options is crucial for managing the disease effectively. Genetic mutations, particularly in enzymes like G6PD, play a significant role in HNSHA. Symptoms can range from mild fatigue to severe anemia, requiring regular medical attention. Treatment often involves managing symptoms through blood transfusions, medications, and sometimes splenectomy. Early diagnosis and genetic counseling can help patients and families navigate this challenging condition. Staying informed and working closely with healthcare providers ensures better management and quality of life for those affected. Remember, knowledge is power when dealing with any medical condition.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
