Erythroplasia of Queyrat might sound like a mouthful, but understanding it is crucial. This condition is a rare form of precancerous lesion that appears on the skin, particularly affecting the genital area. Named after the French dermatologist Louis Queyrat, it primarily targets uncircumcised men. The lesions are usually red, velvety patches that can be mistaken for other skin issues. Early detection is key because these patches can develop into squamous cell carcinoma, a type of skin cancer. Knowing the symptoms, risk factors, and treatment options can make a significant difference in outcomes. Let's dive into 40 essential facts about Erythroplasia of Queyrat to arm you with the knowledge you need.
Key Takeaways:
- Erythroplasia of Queyrat is a rare form of skin cancer that primarily affects the genital area in men. Early detection and treatment are crucial for better outcomes.
- Prevention strategies such as good genital hygiene, regular medical check-ups, and HPV vaccination can significantly reduce the risk of developing Erythroplasia of Queyrat.
What is Erythroplasia of Queyrat?
Erythroplasia of Queyrat is a rare but significant medical condition. It primarily affects the skin of the genital area, particularly in men. Understanding this condition is crucial for early detection and treatment.
- Erythroplasia of Queyrat is a type of squamous cell carcinoma in situ, meaning it is a form of skin cancer that has not yet spread beyond the surface layer of the skin.
- This condition was first described by the French dermatologist Louis Queyrat in 1911.
- It typically appears as a red, velvety patch on the glans penis or the inner foreskin.
- Erythroplasia of Queyrat is more common in uncircumcised men.
- The exact cause is unknown, but it is often linked to human papillomavirus (HPV) infection.
Symptoms and Diagnosis
Recognizing the symptoms early can lead to better outcomes. Diagnosis usually involves a combination of physical examination and biopsy.
- Symptoms include persistent redness, irritation, and sometimes itching or burning in the affected area.
- The lesion may bleed or ulcerate if left untreated.
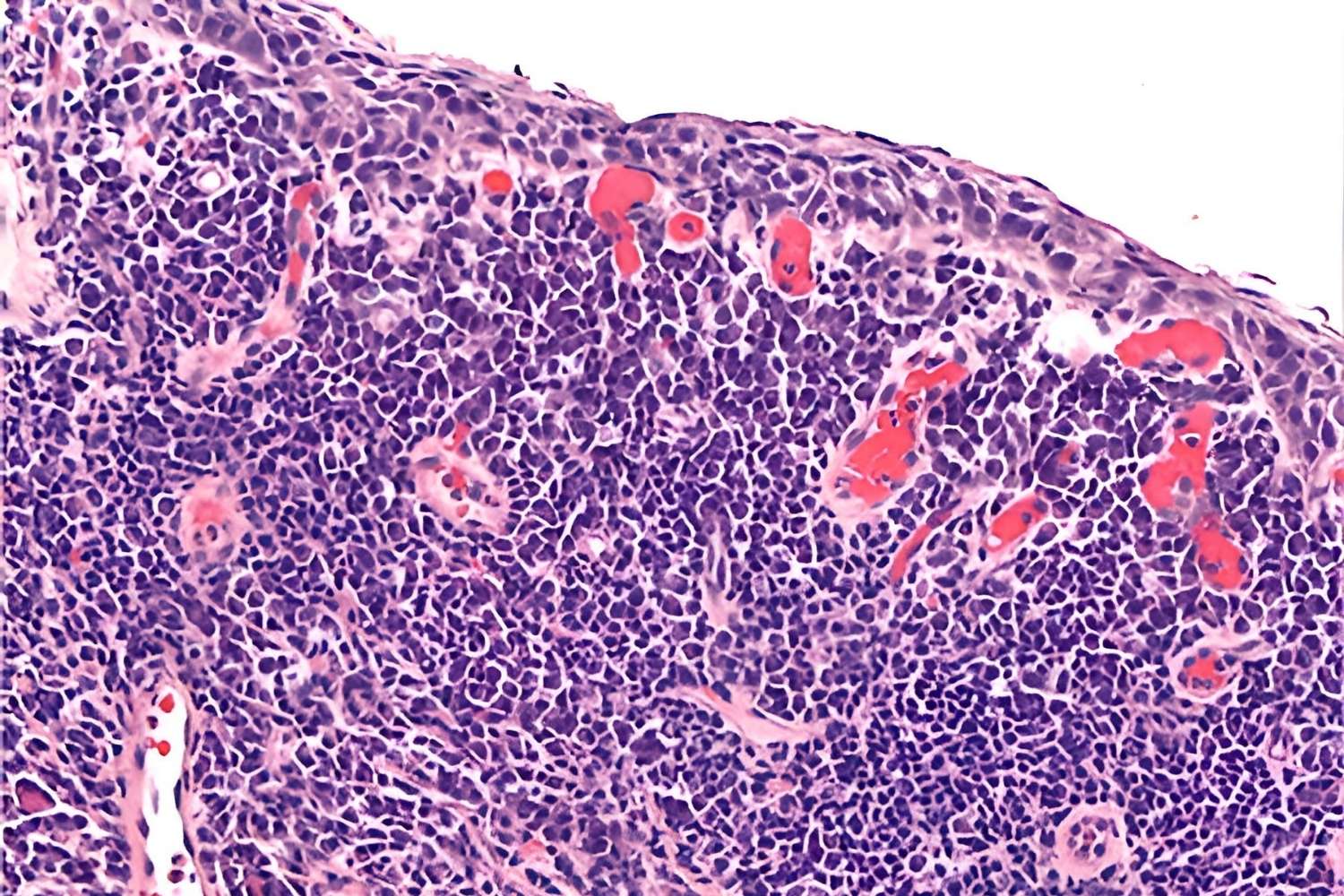
- A biopsy is essential for diagnosis, where a small tissue sample is examined under a microscope.
- Dermoscopy, a non-invasive skin imaging technique, can help in the initial assessment.
- Misdiagnosis is common, as it can resemble other conditions like balanitis or psoriasis.
Risk Factors
Certain factors can increase the likelihood of developing Erythroplasia of Queyrat. Awareness of these can aid in prevention and early detection.
- Chronic irritation or inflammation of the genital area is a significant risk factor.
- Poor hygiene practices can contribute to the development of this condition.
- Immunosuppressed individuals, such as those with HIV/AIDS, are at higher risk.
- Men over the age of 50 are more commonly affected.
- Smoking has been linked to an increased risk of developing Erythroplasia of Queyrat.
Treatment Options
Various treatment options are available, ranging from topical therapies to surgical interventions. The choice depends on the lesion's size, location, and severity.
- Topical chemotherapy with 5-fluorouracil is often used to treat small lesions.
- Imiquimod cream, an immune response modifier, can also be effective.
- Laser therapy, particularly CO2 laser, is another treatment option.
- Cryotherapy, which involves freezing the lesion, can be used for smaller areas.
- Surgical excision may be necessary for larger or more persistent lesions.
Prognosis and Follow-Up
The prognosis for Erythroplasia of Queyrat is generally good with early treatment. However, regular follow-up is essential to monitor for recurrence.
- The five-year survival rate is high when treated early.
- Recurrence is possible, so regular follow-up visits are crucial.
- Patients should perform regular self-examinations to detect any new lesions.
- Photodynamic therapy, which uses light to activate a photosensitizing agent, can be used for recurrent cases.
- In rare cases, untreated Erythroplasia of Queyrat can progress to invasive squamous cell carcinoma.
Prevention and Awareness
Prevention strategies and awareness can significantly reduce the incidence of Erythroplasia of Queyrat. Education and lifestyle changes play a vital role.
- Practicing good genital hygiene can help prevent this condition.
- Regular medical check-ups can aid in early detection.
- HPV vaccination may reduce the risk of developing Erythroplasia of Queyrat.
- Avoiding smoking can lower the risk.
- Educating men about the symptoms and risks can lead to earlier diagnosis and treatment.
Historical and Medical Significance
Understanding the historical context and medical significance of Erythroplasia of Queyrat provides insight into its impact on health.
- Louis Queyrat's initial description in 1911 paved the way for further research and understanding.
- The condition is named after Queyrat to honor his contributions to dermatology.
- Erythroplasia of Queyrat is considered a precursor to invasive penile cancer.
- Research continues to explore the links between HPV and this condition.
- Advances in medical imaging and biopsy techniques have improved diagnosis accuracy.
Patient Stories and Experiences
Hearing from those who have experienced Erythroplasia of Queyrat can provide valuable insights and support for others.
- Many patients report initial misdiagnosis, highlighting the need for awareness.
- Successful treatment stories emphasize the importance of early detection.
- Support groups and online forums can offer emotional support and information.
- Sharing experiences can help reduce the stigma associated with genital conditions.
- Patient advocacy plays a crucial role in raising awareness and funding for research.
Key Takeaways on Erythroplasia of Queyrat
Erythroplasia of Queyrat is a rare but serious condition affecting the skin of the genital area. Early detection is crucial for effective treatment. Symptoms include red, velvety patches that may bleed or become ulcerated. Risk factors include HPV infection, poor hygiene, and chronic irritation. Diagnosis often involves a biopsy to confirm the presence of abnormal cells. Treatment options range from topical medications to surgical removal, depending on the severity. Regular follow-ups are essential to monitor for recurrence. Awareness and education can help in early identification and management. If you notice any unusual changes in your genital area, consult a healthcare provider promptly. Taking preventive measures, such as practicing good hygiene and safe sex, can reduce the risk. Stay informed and proactive about your health to ensure the best outcomes.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
