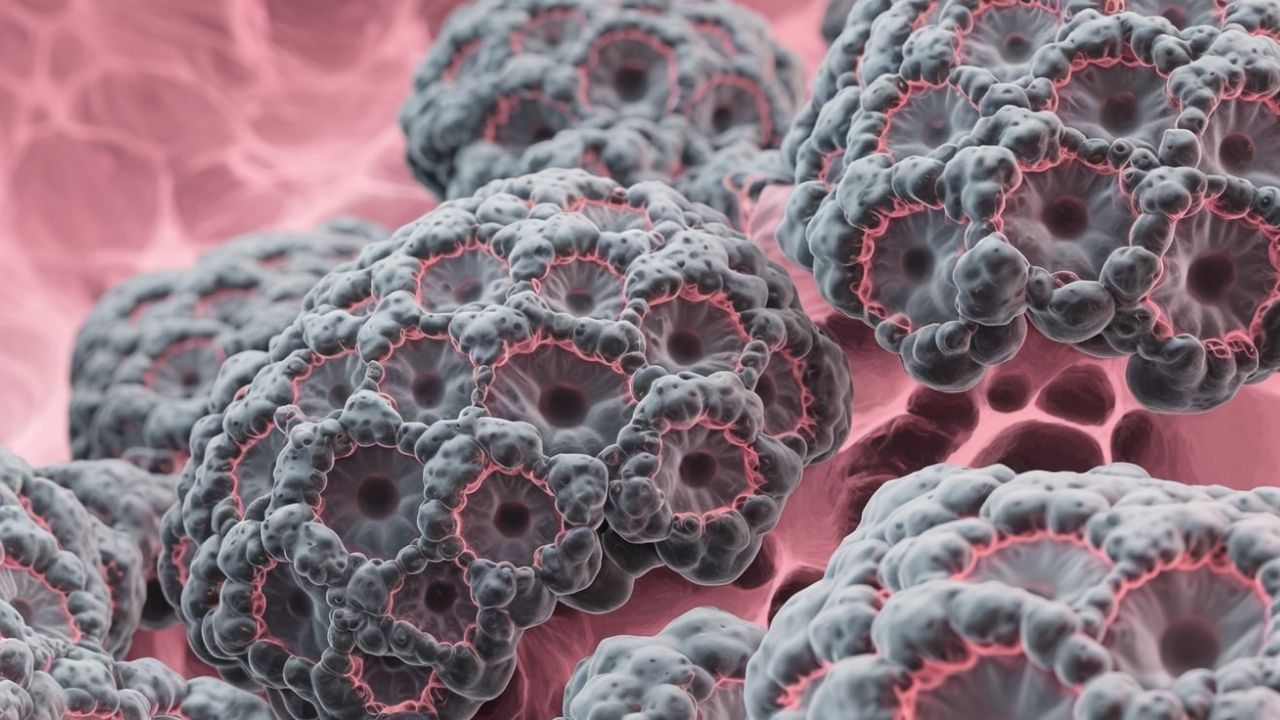
Gastro-Enteropancreatic Neuroendocrine Tumors (GEP-NETs) are rare, complex cancers that develop in the digestive system and pancreas. These tumors can be tricky to diagnose because their symptoms often mimic other conditions. What exactly are GEP-NETs? They are a type of neuroendocrine tumor that originates from cells in the gastrointestinal tract or pancreas. These cells have traits of both nerve cells and hormone-producing cells, making the tumors unique. Understanding GEP-NETs is crucial for early detection and treatment. This article will provide 30 essential facts about GEP-NETs, covering everything from symptoms and diagnosis to treatment options and prognosis. Whether you're a patient, caregiver, or just curious, these facts will help you grasp the basics of this rare condition.
Key Takeaways:
- Gastro-Enteropancreatic Neuroendocrine Tumors (GEP-NETs) can be benign or cancerous, affecting the stomach, intestines, and pancreas. Early detection and treatment significantly improve outcomes, with surgery, medication, and regular monitoring as key components.
- Understanding the risk factors and symptoms of GEP-NETs can aid in prevention and early detection. Lifestyle adjustments, emotional support, and staying informed about new treatments are crucial for managing the disease and leading a fulfilling life.
What is a Gastro-Enteropancreatic Neuroendocrine Tumor?
Gastro-enteropancreatic neuroendocrine tumors (GEP-NETs) are rare and complex. They originate in the neuroendocrine cells of the gastrointestinal tract and pancreas. Understanding these tumors can help in early detection and treatment.
- GEP-NETs are a type of neuroendocrine tumor that can occur in the stomach, intestines, and pancreas.
- These tumors can be benign or malignant, meaning they can be non-cancerous or cancerous.
- GEP-NETs are often slow-growing, but some can be aggressive and spread quickly.
- They are more common in people aged 50 to 60 years old.
- Symptoms can vary widely depending on the tumor's location and size.
Symptoms and Diagnosis
Recognizing the symptoms of GEP-NETs can be challenging due to their variability. Diagnosis often involves multiple tests and imaging techniques.
- Common symptoms include abdominal pain, diarrhea, and weight loss.
- Some GEP-NETs produce hormones that cause specific symptoms like flushing or wheezing.
- Blood tests can detect elevated hormone levels indicative of GEP-NETs.
- Imaging techniques like CT scans, MRIs, and PET scans help locate and assess the tumor.
- Biopsies are often necessary to confirm the diagnosis and determine the tumor's type and grade.
Treatment Options
Treatment for GEP-NETs depends on the tumor's size, location, and whether it has spread. Options range from surgery to medication.
- Surgery is the primary treatment for localized GEP-NETs and aims to remove the tumor completely.
- For tumors that have spread, debulking surgery can reduce the tumor burden.
- Medications like somatostatin analogs can help control hormone-related symptoms.
- Targeted therapies and chemotherapy may be used for advanced GEP-NETs.
- Peptide receptor radionuclide therapy (PRRT) is a newer treatment that delivers radiation directly to the tumor cells.
Prognosis and Survival Rates
The prognosis for GEP-NETs varies widely based on several factors. Early detection and treatment significantly improve outcomes.
- The five-year survival rate for localized GEP-NETs is around 90%.
- If the tumor has spread to nearby tissues, the five-year survival rate drops to about 70%.
- For metastatic GEP-NETs, the five-year survival rate is approximately 20%.
- Regular follow-ups and monitoring are crucial for managing the disease and detecting recurrences.
- Advances in treatment have improved survival rates and quality of life for many patients.
Risk Factors and Prevention
Understanding the risk factors for GEP-NETs can aid in prevention and early detection. While some factors are unavoidable, others can be managed.
- Genetic conditions like Multiple Endocrine Neoplasia type 1 (MEN1) increase the risk of developing GEP-NETs.
- Family history of neuroendocrine tumors can also be a significant risk factor.
- Chronic conditions like gastritis and Zollinger-Ellison syndrome are associated with a higher risk of GEP-NETs.
- Smoking and excessive alcohol consumption may contribute to the development of these tumors.
- Regular screenings and genetic counseling can help those at high risk.
Living with GEP-NETs
Managing life with GEP-NETs involves medical treatment, lifestyle adjustments, and emotional support. Patients can lead fulfilling lives with proper care.
- A balanced diet and regular exercise can help manage symptoms and improve overall health.
- Support groups and counseling can provide emotional support and practical advice.
- Regular medical check-ups are essential for monitoring the disease and adjusting treatment plans.
- Patients should stay informed about new treatments and clinical trials that may offer additional options.
- Open communication with healthcare providers ensures that patients receive comprehensive care tailored to their needs.
Final Thoughts on Gastro-Enteropancreatic Neuroendocrine Tumors
Gastro-Enteropancreatic Neuroendocrine Tumors (GEP-NETs) are rare but significant. Understanding these tumors can help in early detection and treatment. GEP-NETs often present with vague symptoms, making diagnosis tricky. However, advancements in medical imaging and biomarkers have improved detection rates. Treatment options vary from surgery to targeted therapies, offering hope for many patients. Awareness and research are crucial in combating these tumors. By staying informed, patients and caregivers can make better decisions and advocate for effective treatments. Remember, knowledge is power when dealing with GEP-NETs. Stay proactive, consult healthcare professionals, and support ongoing research efforts.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
