Peripheral Type Neurofibromatosis, also known as Neurofibromatosis Type 1 (NF1), is a genetic disorder that affects the nervous system. This condition causes tumors to form on nerve tissues, leading to skin changes, bone deformities, and other complications. NF1 is one of the most common inherited neurological disorders, affecting about 1 in 3,000 people worldwide. Symptoms can vary widely, even among family members. Some individuals may have mild symptoms, while others experience severe complications. Understanding NF1 is crucial for managing its effects and improving quality of life. Here are 50 facts to help you grasp the essentials of this complex condition.
Key Takeaways:
- Neurofibromatosis Type 1 (NF1) is a genetic disorder causing benign tumors. It affects 1 in 3,000 people and can lead to skin spots, learning disabilities, and other complications.
- Living with NF1 can be challenging, but support groups, medical check-ups, and healthy lifestyle choices can improve quality of life. Family and mental health support are crucial for individuals with NF1.
What is Peripheral Type Neurofibromatosis?
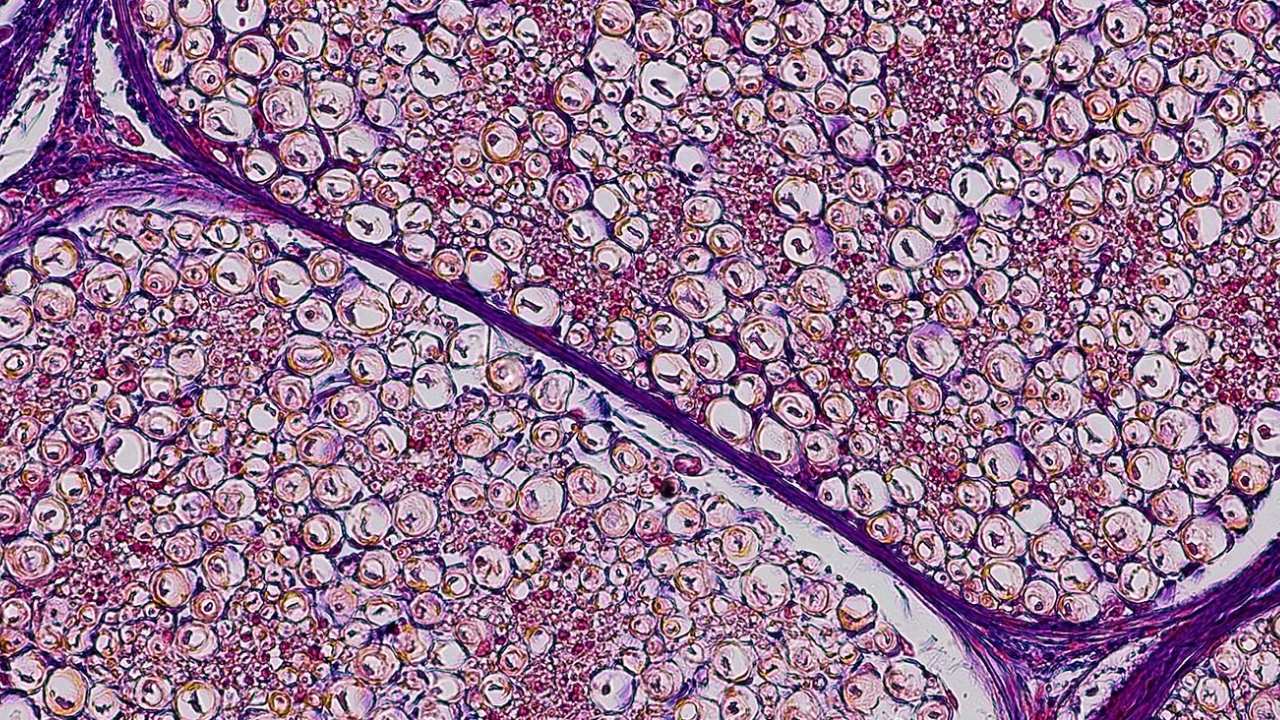
Peripheral Type Neurofibromatosis, also known as Neurofibromatosis Type 1 (NF1), is a genetic disorder that primarily affects the skin and peripheral nervous system. It is characterized by the development of multiple benign tumors called neurofibromas. Let's dive into some fascinating facts about this condition.
-
NF1 is a genetic disorder caused by mutations in the NF1 gene located on chromosome 17.
-
It affects approximately 1 in 3,000 people worldwide, making it one of the most common genetic disorders.
-
NF1 is inherited in an autosomal dominant manner, meaning only one copy of the mutated gene is needed to develop the disorder.
-
About 50% of cases are due to new mutations, meaning they occur spontaneously without a family history.
-
Café-au-lait spots are a hallmark of NF1, appearing as light brown patches on the skin.
-
Neurofibromas can develop anywhere in the body, including under the skin, along nerves, and even in internal organs.
-
Plexiform neurofibromas are a more complex type of tumor that can cause significant disfigurement and functional impairment.
-
Lisch nodules are another common feature, appearing as tiny, benign growths on the iris of the eye.
-
Scoliosis, or curvature of the spine, is a frequent complication in individuals with NF1.
-
Learning disabilities affect up to 50% of children with NF1, often requiring special educational support.
Symptoms and Diagnosis of NF1
Understanding the symptoms and how NF1 is diagnosed can help in early detection and management. Here are some key points to consider.
-
Freckling in the armpits or groin area is another diagnostic criterion for NF1.
-
Optic gliomas, or tumors of the optic nerve, can lead to vision problems and are common in children with NF1.
-
Bone abnormalities, such as tibial dysplasia, can cause bowing of the legs and fractures.
-
Macrocephaly, or an unusually large head, is often observed in individuals with NF1.
-
A diagnosis is typically made based on clinical criteria, including the presence of two or more characteristic features.
-
Genetic testing can confirm the diagnosis, especially in uncertain cases or for prenatal diagnosis.
-
Regular monitoring by a multidisciplinary team is essential for managing the various complications of NF1.
-
MRI scans are often used to detect internal tumors and monitor their growth.
-
Skin biopsies may be performed to examine suspicious lesions more closely.
-
Early intervention can improve quality of life, particularly for children with learning disabilities or physical deformities.
Treatment and Management of NF1
While there is no cure for NF1, various treatments and management strategies can help alleviate symptoms and improve quality of life.
-
Surgical removal of neurofibromas is sometimes necessary, especially if they cause pain or functional impairment.
-
Radiation therapy may be used for certain types of tumors, although it carries risks of secondary malignancies.
-
Chemotherapy is an option for aggressive tumors, such as malignant peripheral nerve sheath tumors.
-
Physical therapy can help manage scoliosis and other musculoskeletal issues.
-
Occupational therapy is beneficial for children with learning disabilities and developmental delays.
-
Regular eye exams are crucial for detecting and managing optic gliomas.
-
Pain management strategies include medications, physical therapy, and sometimes surgery.
-
Psychological support is important, as individuals with NF1 may experience anxiety, depression, and social isolation.
-
Genetic counseling can provide valuable information for affected individuals and their families.
-
Clinical trials offer access to new treatments, and participation can contribute to advancing research.
Research and Future Directions
Ongoing research is crucial for understanding NF1 better and developing new treatments. Here are some exciting developments in the field.
-
The NF1 gene was identified in 1990, a significant milestone in understanding the disorder.
-
Animal models, such as mice with NF1 mutations, are used to study the disease and test new treatments.
-
Researchers are exploring targeted therapies, which aim to block specific pathways involved in tumor growth.
-
Gene therapy holds promise for correcting the underlying genetic defect in NF1.
-
Clinical trials are investigating the use of MEK inhibitors, a class of drugs that may shrink neurofibromas.
-
Stem cell research is another area of interest, with potential applications for regenerating damaged tissues.
-
Advances in imaging techniques are improving the detection and monitoring of tumors.
-
Patient registries and biobanks are valuable resources for researchers studying NF1.
-
Collaborative research efforts, such as the Neurofibromatosis Therapeutic Acceleration Program, are accelerating progress.
-
Public awareness campaigns are helping to reduce stigma and improve understanding of NF1.
Living with NF1
Living with NF1 can be challenging, but many individuals lead fulfilling lives with proper support and management.
-
Support groups provide a sense of community and valuable resources for individuals and families affected by NF1.
-
Educational accommodations can help children with learning disabilities succeed in school.
-
Regular medical check-ups are essential for monitoring and managing complications.
-
Healthy lifestyle choices, such as a balanced diet and regular exercise, can improve overall well-being.
-
Advocacy organizations, like the Children's Tumor Foundation, offer support and resources for those affected by NF1.
-
Mental health support is crucial, as living with a chronic condition can be emotionally taxing.
-
Employment accommodations may be necessary for individuals with physical or cognitive impairments.
-
Adaptive devices and technologies can enhance independence and quality of life.
-
Family and friends play a vital role in providing emotional and practical support.
-
Staying informed about the latest research and treatments empowers individuals to make informed decisions about their care.
Final Thoughts on Peripheral Type Neurofibromatosis
Peripheral Type Neurofibromatosis, or NF1, is a complex condition affecting many people worldwide. Understanding its symptoms, causes, and treatments can help those diagnosed manage their condition better. Early detection and regular monitoring are crucial for managing NF1 effectively. Genetic counseling can provide valuable insights for families with a history of NF1. While there is no cure yet, ongoing research offers hope for better treatments in the future. Staying informed and connected with support groups can make a significant difference in the lives of those affected. Remember, knowledge is power. The more you know about NF1, the better equipped you'll be to handle its challenges. Keep learning, stay proactive, and support each other.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
