Idiopathic Sclerosing Mesenteritis is a rare and mysterious condition that affects the mesentery, a fold of tissue in the abdomen. This disorder causes inflammation and fibrosis, leading to a thickening of the mesentery. What makes it unique is that its cause remains unknown, hence the term "idiopathic." Symptoms can vary widely, from abdominal pain and bloating to weight loss and fever. Diagnosing this condition can be tricky due to its rarity and the similarity of its symptoms to other abdominal diseases. Treatment often involves medications to reduce inflammation and manage symptoms. Understanding this condition better can help those affected and their families navigate its challenges.
Key Takeaways:
- Idiopathic Sclerosing Mesenteritis is a rare disease causing chronic inflammation in the abdomen, leading to symptoms like pain, bloating, and weight loss. Early detection and tailored treatments are crucial for managing the condition effectively.
- Ongoing research and collaboration aim to better understand Idiopathic Sclerosing Mesenteritis and develop more effective treatments. Increased awareness and patient participation in research are essential for continued advancements in managing the disease.
What is Idiopathic Sclerosing Mesenteritis?
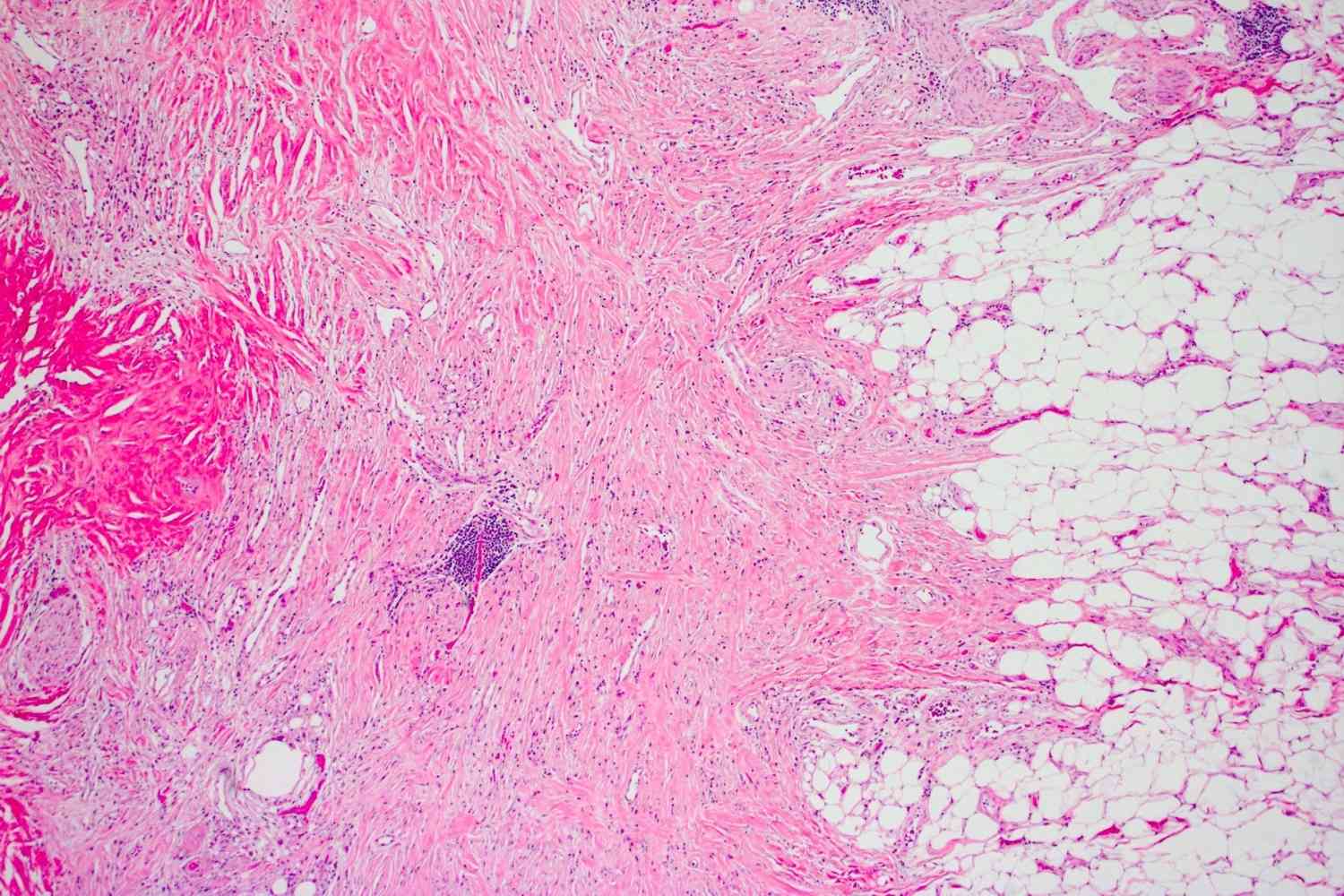
Idiopathic Sclerosing Mesenteritis (ISM) is a rare disorder affecting the mesentery, a fold of tissue attaching the intestines to the abdominal wall. This condition involves chronic inflammation and fibrosis, leading to various symptoms and complications.
- ISM is a rare disease, with fewer than 300 cases reported worldwide.
- The term "idiopathic" means the cause is unknown.
- It primarily affects the mesentery, the tissue connecting the intestines to the abdominal wall.
- ISM can lead to chronic inflammation and fibrosis.
- Symptoms often include abdominal pain, bloating, and weight loss.
- The disease can mimic other conditions, making diagnosis challenging.
- ISM is more common in men than women.
- Most patients are diagnosed between the ages of 50 and 60.
- The exact cause of ISM remains unknown.
- Some researchers believe it may be linked to autoimmune disorders.
Symptoms and Diagnosis
Understanding the symptoms and how ISM is diagnosed can help in managing the condition effectively. Early detection is crucial for better outcomes.
- Abdominal pain is the most common symptom of ISM.
- Patients may experience bloating and a feeling of fullness.
- Weight loss is another frequent symptom.
- Nausea and vomiting can occur in some cases.
- Diarrhea or constipation may also be present.
- Blood tests often show elevated inflammatory markers.
- Imaging studies like CT scans and MRIs are used for diagnosis.
- A biopsy of the mesentery may be required to confirm ISM.
- ISM can be mistaken for other conditions like lymphoma or Crohn's disease.
- Delayed diagnosis can lead to complications such as bowel obstruction.
Treatment Options
While there is no cure for ISM, various treatments can help manage symptoms and improve quality of life. Treatment plans are often tailored to individual needs.
- Corticosteroids are commonly used to reduce inflammation.
- Immunosuppressive drugs may be prescribed in severe cases.
- Surgery might be necessary to remove fibrotic tissue.
- Pain management is crucial for improving patient comfort.
- Dietary changes can help manage symptoms like bloating and nausea.
- Physical therapy may be beneficial for maintaining mobility.
- Regular follow-ups with a gastroenterologist are essential.
- Some patients may benefit from psychological support or counseling.
- Experimental treatments are being researched to find more effective options.
- Early intervention can prevent complications and improve outcomes.
Complications and Prognosis
Understanding the potential complications and long-term outlook for ISM can help patients and caregivers prepare for the future.
- Bowel obstruction is a serious complication of ISM.
- Chronic pain can significantly impact quality of life.
- Malnutrition may occur due to difficulty eating and absorbing nutrients.
- Some patients develop secondary infections from weakened immune systems.
- ISM can lead to the formation of scar tissue in the abdomen.
- The prognosis varies widely among patients.
- Some individuals experience periods of remission.
- Others may have a more progressive course with worsening symptoms.
- Regular monitoring is essential to catch complications early.
- Support groups can provide valuable resources and emotional support.
Research and Future Directions
Ongoing research aims to better understand ISM and develop more effective treatments. Staying informed about the latest advancements can offer hope to patients and their families.
- Researchers are investigating the genetic factors involved in ISM.
- Studies are exploring the role of the immune system in the disease.
- New imaging techniques are being developed for earlier diagnosis.
- Clinical trials are testing novel medications for ISM.
- Patient registries are being created to collect data and improve understanding.
- Collaboration between researchers worldwide is crucial for progress.
- Advances in personalized medicine may lead to more tailored treatments.
- Increased awareness can lead to earlier diagnosis and better outcomes.
- Funding for ISM research is essential for continued advancements.
- Patients and caregivers can contribute to research by participating in studies and sharing their experiences.
Final Thoughts on Idiopathic Sclerosing Mesenteritis
Idiopathic Sclerosing Mesenteritis is a rare, complex condition affecting the mesentery. Understanding its symptoms, causes, and treatment options can help those diagnosed manage their health better. While the exact cause remains unknown, early detection and treatment can significantly improve quality of life. Regular check-ups, a healthy lifestyle, and staying informed about new research are crucial.
Doctors often recommend a combination of medications, including corticosteroids and immunosuppressants, to manage inflammation and symptoms. Surgery might be necessary in severe cases. Support from family, friends, and patient communities can make a big difference in coping with this condition.
Staying proactive about health and seeking medical advice when symptoms arise are key steps. Knowledge empowers patients to make informed decisions and advocate for their well-being. Keep learning, stay vigilant, and prioritize health to navigate the challenges of Idiopathic Sclerosing Mesenteritis effectively.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
