Hyperammonemia might sound like a complex term, but it simply refers to having too much ammonia in the blood. Why is this important? Because ammonia is toxic to the brain, and high levels can lead to serious health issues. This condition can affect anyone, from newborns to adults, and understanding it is crucial for maintaining good health. Causes range from genetic disorders to liver problems, and symptoms can include confusion, fatigue, and even coma. Treatment often involves medications and dietary changes to reduce ammonia levels. Can it be managed? Yes, with early diagnosis and proper care, many people live healthy lives. Learning about hyperammonemia helps in recognizing symptoms early and seeking timely medical attention. Let's explore 50 intriguing facts about this condition to better understand its impact and management.
Key Takeaways:
- Hyperammonemia is a serious condition caused by high ammonia levels in the blood, leading to symptoms like confusion and coma. Early diagnosis and treatment are crucial for preventing complications.
- Treatment for hyperammonemia includes dietary changes, medications, and even liver transplants in severe cases. It's important to monitor at-risk individuals and educate patients and families for early intervention.
What is Hyperammonemia?
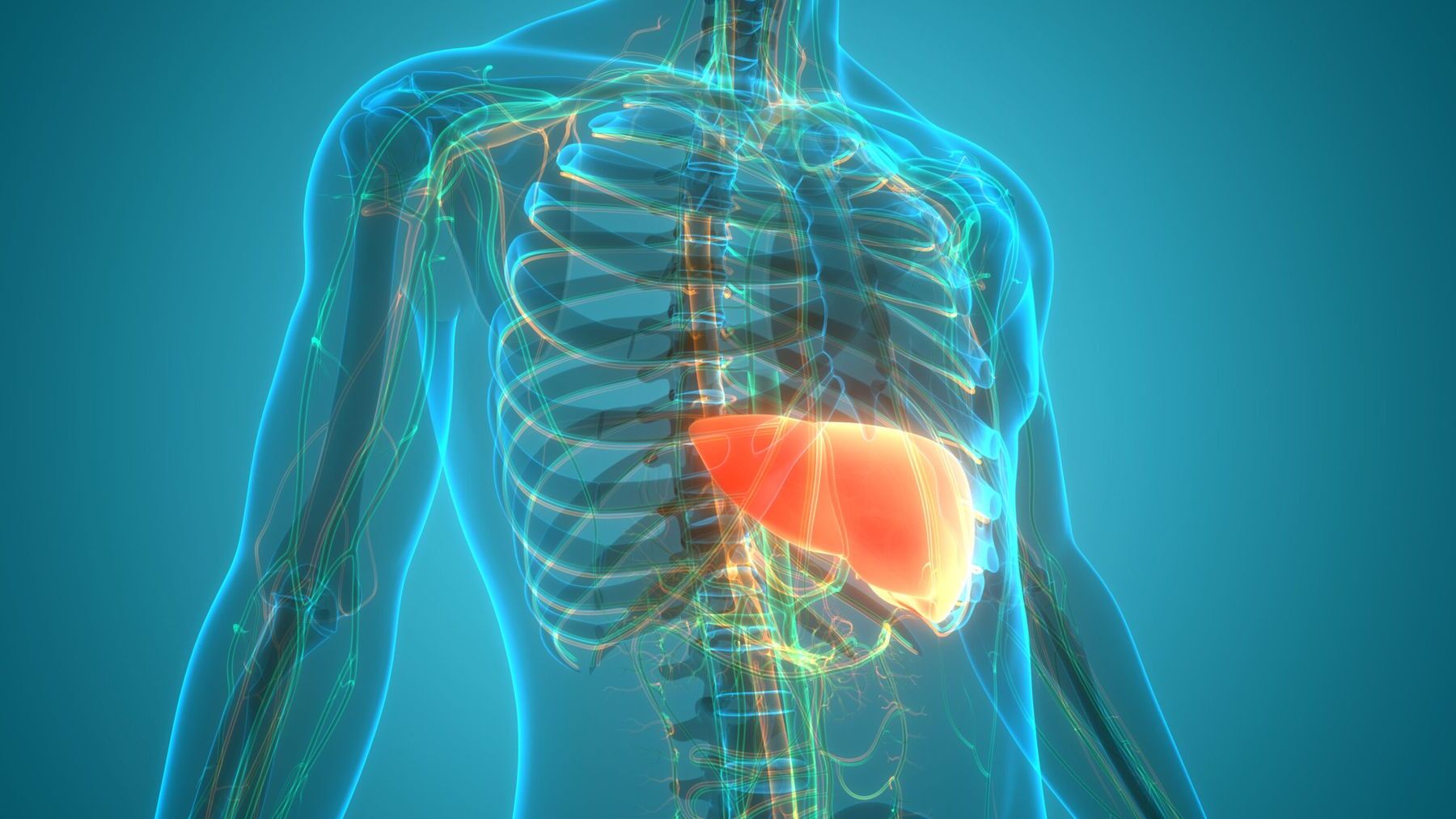
Hyperammonemia is a medical condition characterized by elevated levels of ammonia in the blood. Ammonia is a waste product formed during the digestion of proteins. Normally, the liver converts ammonia into urea, which is then excreted through urine. When this process is disrupted, ammonia accumulates, leading to potential health issues.
-
Ammonia's Role: Ammonia is a byproduct of protein metabolism. It is toxic in high amounts, so the body must efficiently convert it to urea.
-
Liver's Function: The liver plays a crucial role in detoxifying ammonia. Any liver dysfunction can lead to hyperammonemia.
-
Symptoms: Symptoms include confusion, lethargy, and in severe cases, coma. These symptoms arise because ammonia affects brain function.
-
Causes: Causes range from liver disease to genetic disorders affecting the urea cycle.
-
Urea Cycle Disorders: These are genetic conditions where the body cannot effectively convert ammonia to urea, leading to accumulation.
How is Hyperammonemia Diagnosed?
Diagnosing hyperammonemia involves a combination of clinical evaluation and laboratory tests. Early detection is vital to prevent severe complications.
-
Blood Tests: Blood tests measure ammonia levels. Elevated levels indicate hyperammonemia.
-
Liver Function Tests: These tests assess the liver's ability to process ammonia.
-
Genetic Testing: In cases of suspected urea cycle disorders, genetic testing can identify specific mutations.
-
Neurological Assessment: Since ammonia affects the brain, a neurological exam helps assess the impact.
-
Family History: A detailed family history can reveal hereditary patterns, especially in genetic disorders.
Treatment Options for Hyperammonemia
Treatment focuses on reducing ammonia levels and addressing the underlying cause. Timely intervention can prevent serious complications.
-
Dietary Management: Reducing protein intake can lower ammonia production.
-
Medications: Certain medications help remove ammonia from the bloodstream.
-
Liver Transplant: In severe cases, a liver transplant may be necessary to restore normal ammonia processing.
-
Dialysis: Dialysis can rapidly reduce ammonia levels in acute cases.
-
Gene Therapy: Emerging treatments like gene therapy offer hope for genetic causes of hyperammonemia.
Complications Associated with Hyperammonemia
If left untreated, hyperammonemia can lead to severe complications, affecting multiple organ systems.
-
Brain Damage: High ammonia levels can cause irreversible brain damage.
-
Seizures: Ammonia toxicity can trigger seizures.
-
Coma: In extreme cases, patients may fall into a coma.
-
Respiratory Failure: Severe hyperammonemia can lead to respiratory issues.
-
Death: Without treatment, hyperammonemia can be fatal.
Prevention and Management Strategies
Preventing hyperammonemia involves managing risk factors and monitoring at-risk individuals.
-
Regular Monitoring: For those with liver disease or genetic predispositions, regular monitoring is crucial.
-
Lifestyle Changes: Avoiding alcohol and maintaining a healthy diet supports liver function.
-
Genetic Counseling: Families with a history of urea cycle disorders can benefit from genetic counseling.
-
Education: Educating patients and families about symptoms and management can lead to early intervention.
-
Research: Ongoing research aims to improve treatment and prevention strategies.
Interesting Facts About Hyperammonemia
Beyond the medical aspects, hyperammonemia has intriguing facets worth exploring.
-
Historical Cases: Historical records show cases of hyperammonemia before modern medicine understood its cause.
-
Animal Studies: Research in animals has provided insights into ammonia metabolism.
-
Biochemical Pathways: The urea cycle is a complex biochemical pathway involving multiple enzymes.
-
Rare Disorders: Some urea cycle disorders are extremely rare, affecting only a handful of individuals worldwide.
-
Ammonia's Dual Role: While toxic in excess, ammonia is essential for certain cellular processes.
Hyperammonemia in Different Populations
Hyperammonemia can affect individuals differently based on age, genetics, and health status.
-
Newborns: Newborns with urea cycle disorders can present with hyperammonemia shortly after birth.
-
Elderly: Liver function declines with age, increasing the risk of hyperammonemia in the elderly.
-
Athletes: High-protein diets in athletes can lead to increased ammonia production.
-
Pregnant Women: Pregnancy can exacerbate liver conditions, raising ammonia levels.
-
Chronic Illness: Individuals with chronic liver disease are at higher risk.
The Future of Hyperammonemia Research
Advancements in medical research continue to improve our understanding and treatment of hyperammonemia.
-
Biomarkers: Identifying biomarkers can aid in early detection and monitoring.
-
New Medications: Research is ongoing to develop more effective medications with fewer side effects.
-
Personalized Medicine: Tailoring treatment to individual genetic profiles offers promise.
-
Stem Cell Therapy: Stem cell research may provide new avenues for treatment.
-
International Collaboration: Global research efforts are crucial for understanding rare genetic disorders.
Hyperammonemia and Mental Health
The impact of hyperammonemia extends beyond physical health, affecting mental well-being.
-
Cognitive Impairment: Chronic hyperammonemia can lead to long-term cognitive issues.
-
Mood Disorders: Patients may experience mood swings or depression.
-
Support Systems: Mental health support is vital for patients and families.
-
Awareness Campaigns: Raising awareness can reduce stigma and promote understanding.
-
Holistic Care: Integrating mental health care into treatment plans improves outcomes.
Hyperammonemia in Popular Culture
While not commonly featured, hyperammonemia has made appearances in media and literature.
-
Medical Dramas: Some TV shows have depicted cases of hyperammonemia, raising public awareness.
-
Literature: Books on rare diseases occasionally mention hyperammonemia.
-
Documentaries: Documentaries on genetic disorders sometimes explore urea cycle disorders.
-
Patient Stories: Personal stories shared online provide insight into living with hyperammonemia.
-
Advocacy Groups: Organizations advocate for research and support for those affected by hyperammonemia.
Final Thoughts on Hyperammonemia
Hyperammonemia, a condition marked by elevated ammonia levels in the blood, can be a serious health concern. Understanding its causes, symptoms, and treatments is crucial for managing this condition effectively. Liver diseases, genetic disorders, and certain medications can lead to this imbalance. Symptoms like confusion, fatigue, and even coma highlight the importance of early detection and intervention. Treatments often involve dietary changes, medications, and in severe cases, dialysis. Regular monitoring and medical guidance are essential for those at risk. Raising awareness about hyperammonemia can lead to better outcomes and improved quality of life for affected individuals. Staying informed and proactive can make a significant difference. If you or someone you know is experiencing symptoms, seeking medical advice promptly is vital. Knowledge and timely action are key in managing this condition effectively.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
