T-Cell Prolymphocytic Leukemia (T-PLL) is a rare and aggressive type of leukemia that affects mature T-cells. It primarily strikes adults, often around the age of 65. This disease progresses rapidly, making early detection and treatment crucial. Symptoms can include swollen lymph nodes, enlarged spleen, skin rashes, and fatigue. Diagnosing T-PLL involves blood tests, bone marrow biopsies, and imaging studies. Treatment options range from chemotherapy and immunotherapy to stem cell transplants. Despite its rarity, understanding T-PLL is vital for those affected and their families. Knowledge about this condition can lead to better management and improved outcomes.
Key Takeaways:
- T-Cell Prolymphocytic Leukemia is a rare and aggressive type of leukemia that primarily affects older adults, with symptoms including enlarged spleen, swollen lymph nodes, and skin rashes. Early diagnosis and treatment are crucial.
- Research and ongoing clinical trials offer hope for improved treatments and outcomes for T-Cell Prolymphocytic Leukemia, including targeted therapies, immunotherapy, and advances in stem cell transplantation. Collaboration between researchers, clinicians, and patients is essential for progress.
What is T-Cell Prolymphocytic Leukemia?
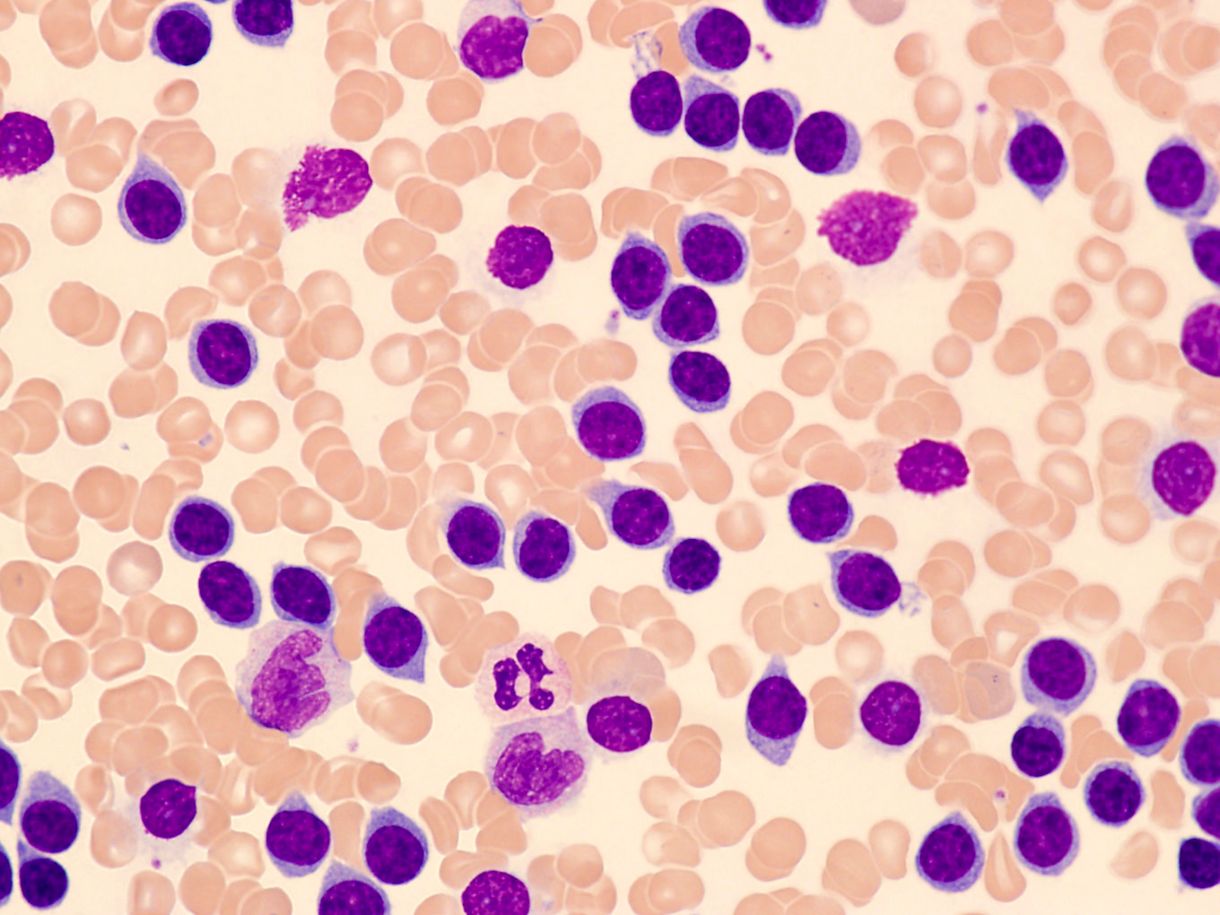
T-Cell Prolymphocytic Leukemia (T-PLL) is a rare and aggressive type of leukemia. It primarily affects adults and involves the overproduction of immature T-cells. Understanding this disease can help in recognizing symptoms and exploring treatment options.
- T-PLL is a type of leukemia that originates from T-cells, a kind of white blood cell crucial for immune response.
- It is considered rare, accounting for less than 2% of all cases of mature lymphocytic leukemia.
- The disease is more common in older adults, typically affecting individuals over the age of 60.
- Men are more frequently diagnosed with T-PLL than women.
- T-PLL progresses rapidly, making early diagnosis and treatment critical.
Symptoms of T-Cell Prolymphocytic Leukemia
Recognizing the symptoms of T-PLL can lead to earlier diagnosis and better management of the disease. Symptoms can vary but often include the following:
- Enlarged spleen (splenomegaly) is a common symptom, causing discomfort or pain in the upper left abdomen.
- Patients may experience swollen lymph nodes, particularly in the neck, armpits, or groin.
- Skin rashes or lesions can appear, often as red or purplish spots.
- Fatigue and general weakness are frequent complaints among those with T-PLL.
- Night sweats and unexplained weight loss are also common symptoms.
Causes and Risk Factors
Understanding the causes and risk factors associated with T-PLL can provide insight into its development and potential prevention strategies.
- The exact cause of T-PLL remains unknown, but genetic mutations are believed to play a significant role.
- Exposure to certain chemicals, such as pesticides, may increase the risk of developing T-PLL.
- A family history of leukemia or other blood disorders can be a risk factor.
- Previous radiation therapy for other cancers might elevate the risk of T-PLL.
- Chronic immune system suppression, such as from organ transplants, can also be a contributing factor.
Diagnosis of T-Cell Prolymphocytic Leukemia
Diagnosing T-PLL involves a series of tests and evaluations to confirm the presence of the disease and determine its extent.
- Blood tests are often the first step, revealing abnormal levels of white blood cells.
- A bone marrow biopsy can provide more detailed information about the type and stage of leukemia.
- Flow cytometry is used to analyze the characteristics of cells in the blood or bone marrow.
- Genetic testing can identify specific mutations associated with T-PLL.
- Imaging tests, such as CT scans, may be used to check for enlarged lymph nodes or spleen.
Treatment Options for T-Cell Prolymphocytic Leukemia
Treatment for T-PLL aims to control the disease and manage symptoms. Options vary based on the patient's overall health and disease progression.
- Chemotherapy is a common treatment, using drugs to kill cancer cells or stop their growth.
- Alemtuzumab, a monoclonal antibody, targets specific proteins on the surface of T-PLL cells.
- Stem cell transplantation may be considered for eligible patients, offering a potential cure.
- Radiation therapy can be used to shrink enlarged organs or lymph nodes.
- Clinical trials may provide access to new and experimental treatments.
Prognosis and Survival Rates
The prognosis for T-PLL can vary widely based on several factors, including the patient's age, overall health, and response to treatment.
- T-PLL generally has a poor prognosis due to its aggressive nature.
- The median survival rate for T-PLL patients is typically less than one year without treatment.
- With treatment, some patients may achieve remission, but relapses are common.
- Younger patients and those who respond well to initial treatment may have better outcomes.
- Ongoing research aims to improve survival rates and develop more effective treatments.
Living with T-Cell Prolymphocytic Leukemia
Managing life with T-PLL involves addressing both physical and emotional challenges. Support and resources can make a significant difference.
- Regular follow-up appointments are essential to monitor the disease and adjust treatment as needed.
- Patients may need to manage side effects from treatments, such as fatigue, nausea, or infections.
- Emotional support from family, friends, or support groups can help cope with the stress of the disease.
- Maintaining a healthy lifestyle, including a balanced diet and regular exercise, can improve overall well-being.
- Palliative care may be necessary to manage symptoms and improve quality of life.
Research and Future Directions
Ongoing research is crucial for understanding T-PLL better and developing new treatments. Scientists and medical professionals continue to explore various aspects of the disease.
- Researchers are investigating the genetic mutations that contribute to T-PLL to develop targeted therapies.
- New drugs and treatment combinations are being tested in clinical trials to improve outcomes.
- Immunotherapy, which harnesses the body's immune system to fight cancer, shows promise for T-PLL.
- Advances in stem cell transplantation techniques may increase the success rates for eligible patients.
- Collaboration between researchers, clinicians, and patients is essential to drive progress in T-PLL treatment and care.
Final Thoughts on T-Cell Prolymphocytic Leukemia
T-Cell Prolymphocytic Leukemia (T-PLL) is a rare, aggressive type of leukemia that primarily affects adults. It’s crucial to understand the symptoms, which can include enlarged spleen, liver, and lymph nodes, as well as skin rashes and high white blood cell counts. Early diagnosis and treatment are vital for managing this disease. Treatment options often involve chemotherapy, immunotherapy, and sometimes stem cell transplants. Research is ongoing, with new therapies being explored to improve patient outcomes. Awareness and education about T-PLL can lead to earlier detection and better support for those affected. If you or a loved one shows symptoms, consult a healthcare professional promptly. Knowledge is power, and staying informed can make a significant difference in the fight against T-PLL.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
