Gestational Trophoblastic Disease (GTD) is a rare group of pregnancy-related tumors. These tumors start in the cells that would normally develop into the placenta during pregnancy. GTD can be benign or malignant, meaning it can spread to other parts of the body. The most common types include hydatidiform mole (complete or partial) and choriocarcinoma. Symptoms often mimic those of a normal pregnancy, making early detection tricky. However, unusual vaginal bleeding, severe nausea, and rapid uterine growth can be warning signs. Early diagnosis and treatment are crucial for a positive outcome. Understanding GTD helps in recognizing symptoms and seeking timely medical advice.
Key Takeaways:
- Gestational Trophoblastic Disease (GTD) is a rare group of pregnancy-related tumors, with symptoms like abnormal vaginal bleeding. Early detection and treatment are crucial for better outcomes.
- Understanding the causes, symptoms, and treatment options for GTD can help women navigate this challenging journey. Support groups and regular medical check-ups are essential for managing GTD.
What is Gestational Trophoblastic Disease?
Gestational Trophoblastic Disease (GTD) is a rare group of pregnancy-related tumors. These tumors originate from the cells that would normally develop into the placenta during pregnancy. Understanding GTD can help in early detection and treatment.
- GTD includes several conditions, such as hydatidiform mole (molar pregnancy) and choriocarcinoma.
- It occurs in about 1 in every 1,000 pregnancies worldwide.
- GTD is more common in women under 20 and over 35.
- Symptoms often include abnormal vaginal bleeding during or after pregnancy.
- GTD can be benign or malignant, with malignant forms requiring more aggressive treatment.
Types of Gestational Trophoblastic Disease
There are different types of GTD, each with unique characteristics and treatment approaches. Knowing these types helps in understanding the disease better.
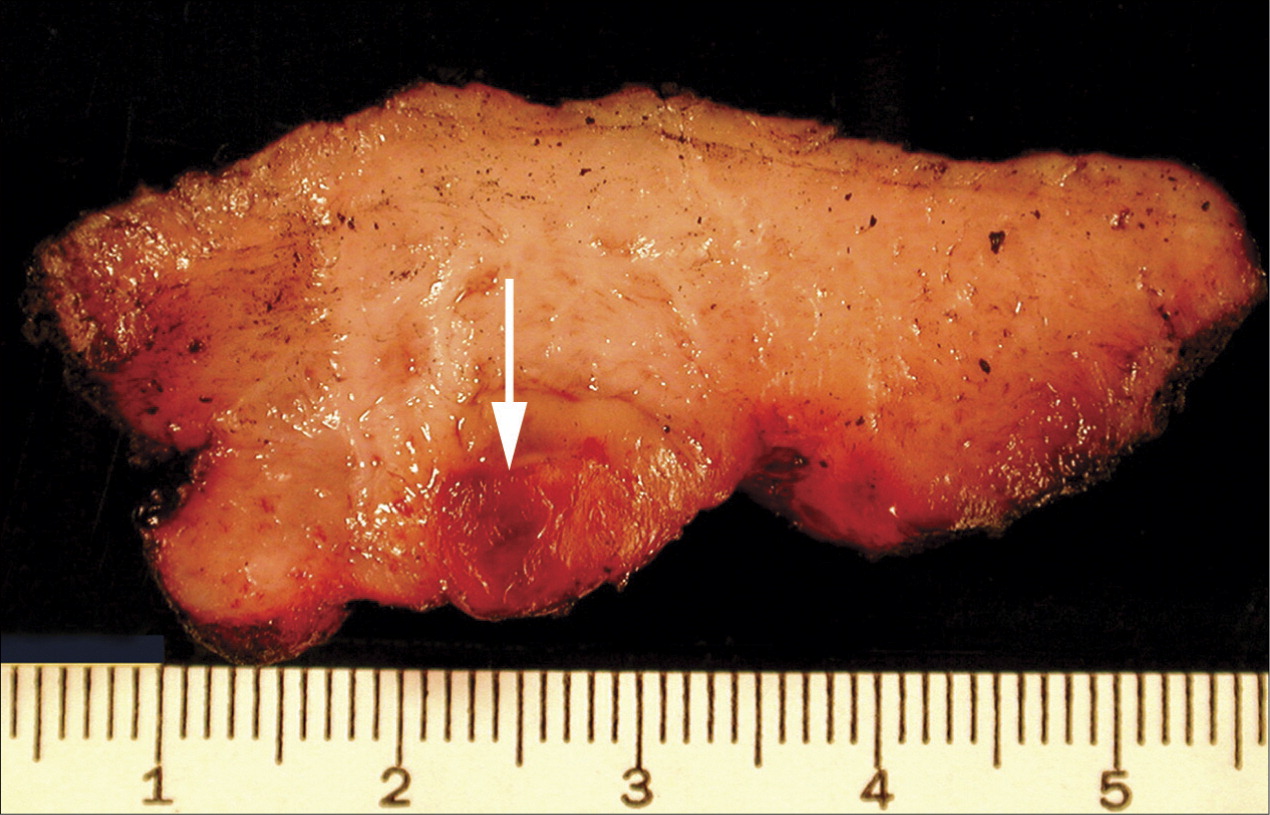
- Hydatidiform mole is the most common type, divided into complete and partial moles.
- Complete moles have no normal fetal tissue, while partial moles have some normal tissue.
- Invasive moles can penetrate the uterine wall and spread to other parts of the body.
- Choriocarcinoma is a highly malignant form of GTD that can spread quickly.
- Placental-site trophoblastic tumor (PSTT) is a rare type that grows where the placenta attaches to the uterus.
Causes and Risk Factors
Understanding the causes and risk factors of GTD can aid in prevention and early diagnosis. While the exact cause is unknown, certain factors increase the risk.
- Previous molar pregnancy increases the risk of GTD in future pregnancies.
- A history of miscarriage can also be a risk factor.
- Women with blood type A or AB have a higher risk compared to those with type O.
- Nutritional deficiencies, particularly low levels of carotene and vitamin A, may contribute to GTD.
- Genetic factors can play a role, with some cases linked to abnormalities in the chromosomes of the sperm or egg.
Symptoms and Diagnosis
Recognizing the symptoms of GTD is crucial for timely diagnosis and treatment. Early detection can significantly improve outcomes.
- Common symptoms include severe nausea and vomiting, often more intense than typical morning sickness.
- Rapid uterine growth, larger than expected for the stage of pregnancy, can be a sign.
- High levels of the pregnancy hormone hCG (human chorionic gonadotropin) are often present.
- Ultrasound imaging can help identify molar pregnancies by showing a "snowstorm" pattern.
- Blood tests measuring hCG levels are essential for diagnosing and monitoring GTD.
Treatment Options
Treatment for GTD varies depending on the type and stage of the disease. Early intervention can lead to successful outcomes.
- Suction curettage is a common procedure to remove molar tissue from the uterus.
- Chemotherapy is often used for malignant forms of GTD, such as choriocarcinoma.
- Methotrexate and dactinomycin are common chemotherapy drugs used in treatment.
- Hysterectomy may be necessary in severe cases or for women who do not wish to preserve fertility.
- Follow-up care includes regular monitoring of hCG levels to ensure the disease has not returned.
Prognosis and Survival Rates
The prognosis for GTD is generally good, especially with early detection and treatment. Survival rates are high for most types of GTD.
- The survival rate for non-metastatic GTD is nearly 100% with appropriate treatment.
- Even metastatic GTD has a high survival rate, around 90%, with aggressive treatment.
- Regular follow-up care is crucial to monitor for recurrence, which can occur in some cases.
- Women who have had GTD can often have normal pregnancies in the future.
- Emotional support and counseling are important for women dealing with the stress of GTD.
Research and Advances
Ongoing research continues to improve the understanding and treatment of GTD. Advances in medical science offer hope for even better outcomes.
- Genetic research is helping to identify specific mutations associated with GTD.
- New imaging techniques are improving early detection and diagnosis.
- Targeted therapies are being developed to treat malignant forms of GTD more effectively.
- Clinical trials are exploring the use of immunotherapy in treating GTD.
- Advances in fertility preservation techniques are helping women maintain the ability to have children after treatment.
Living with Gestational Trophoblastic Disease
Living with GTD can be challenging, but support and resources are available to help women navigate this journey. Understanding the emotional and physical aspects is key.
- Support groups can provide emotional support and practical advice for women with GTD.
- Counseling services can help address the psychological impact of the disease.
- Maintaining a healthy lifestyle, including proper nutrition and exercise, can aid in recovery.
- Regular medical check-ups are essential for monitoring health and preventing recurrence.
- Education and awareness about GTD can empower women to seek timely medical attention and support.
Final Thoughts on Gestational Trophoblastic Disease
Gestational Trophoblastic Disease (GTD) might sound complex, but understanding it can make a big difference. Early detection and treatment are crucial for better outcomes. GTD includes several conditions, from benign moles to malignant cancers. Regular check-ups during pregnancy help catch any issues early. Treatment often involves surgery, chemotherapy, or both, depending on the type and stage. Support from healthcare providers and loved ones is essential for those affected. Awareness and education about GTD can lead to earlier diagnoses and better care. Remember, knowledge is power when it comes to health. Stay informed, ask questions, and seek medical advice if something feels off. GTD is rare, but being aware can save lives.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
