Fitz-Hugh–Curtis Syndrome might sound like a mouthful, but understanding it is crucial for anyone interested in women's health. This rare condition links pelvic inflammatory disease (PID) to liver inflammation, causing sharp pain in the upper right abdomen. Fitz-Hugh–Curtis Syndrome often affects women of childbearing age and can be mistaken for other abdominal issues. Knowing the symptoms, causes, and treatments can help in early diagnosis and better management. This post will dive into 40 essential facts about Fitz-Hugh–Curtis Syndrome, shedding light on its complexities and offering valuable insights for those affected or curious. Ready to learn more? Let's get started!
Key Takeaways:
- Fitz-Hugh–Curtis Syndrome is a rare condition linked to pelvic infections, causing severe abdominal pain in women. Early diagnosis and treatment are crucial for preventing long-term complications.
- Prevention through safe sex practices, regular screenings, and prompt treatment of pelvic infections can reduce the risk of developing Fitz-Hugh–Curtis Syndrome. Education and vaccinations also play a key role in prevention.
What is Fitz-Hugh–Curtis Syndrome?
Fitz-Hugh–Curtis Syndrome (FHCS) is a rare condition that involves inflammation of the liver capsule, often linked to pelvic inflammatory disease (PID). It primarily affects women and can cause significant pain in the upper right abdomen. Here are some intriguing facts about this uncommon syndrome.
-
Named After Two Doctors: The syndrome is named after Dr. Thomas Fitz-Hugh Jr. and Dr. Arthur Curtis, who first described the condition in the 1930s.
-
Associated with PID: FHCS is often associated with pelvic inflammatory disease, which is an infection of the female reproductive organs.
-
Bacterial Infection: The condition is usually caused by bacteria such as Chlamydia trachomatis or Neisseria gonorrhoeae.
-
Symptoms Mimic Other Conditions: Symptoms of FHCS can mimic those of gallbladder disease or liver issues, making diagnosis challenging.
-
Upper Right Abdominal Pain: One of the hallmark symptoms is severe pain in the upper right quadrant of the abdomen.
How is Fitz-Hugh–Curtis Syndrome Diagnosed?
Diagnosing FHCS can be tricky due to its similarity to other abdominal conditions. Here are some key points about the diagnostic process.
-
Medical History: A thorough medical history, including any recent pelvic infections, is crucial for diagnosis.
-
Physical Examination: Doctors often perform a physical exam to check for tenderness in the upper right abdomen.
-
Imaging Tests: Ultrasound or CT scans may be used to rule out other conditions like gallstones or liver disease.
-
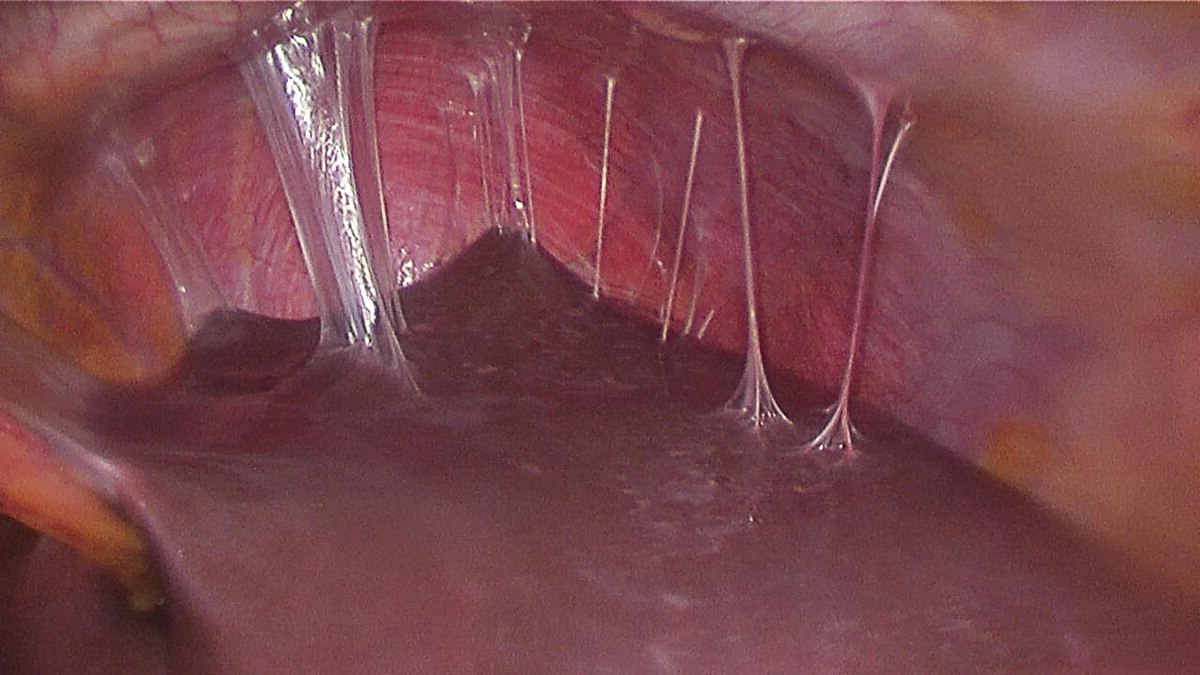
Laparoscopy: In some cases, a laparoscopy is performed to directly visualize the liver and confirm the diagnosis.
-
Blood Tests: Blood tests can help identify the presence of infection or inflammation.
Treatment Options for Fitz-Hugh–Curtis Syndrome
Treatment for FHCS focuses on addressing the underlying infection and managing symptoms. Here are some common treatment methods.
-
Antibiotics: The primary treatment involves antibiotics to eliminate the bacterial infection.
-
Pain Management: Pain relievers may be prescribed to manage abdominal pain.
-
Rest and Hydration: Patients are often advised to rest and stay hydrated to aid recovery.
-
Follow-Up Care: Regular follow-up appointments are essential to ensure the infection has cleared.
-
Surgery: In rare cases, surgery may be needed if there are complications or if the diagnosis is uncertain.
Complications and Long-Term Effects
While FHCS is treatable, it can lead to complications if not addressed promptly. Here are some potential long-term effects.
-
Chronic Pain: Some patients may experience chronic abdominal pain even after treatment.
-
Adhesions: The inflammation can cause adhesions, or scar tissue, to form around the liver.
-
Infertility: If associated with severe PID, there is a risk of infertility.
-
Recurrent Infections: Patients may be at higher risk for recurrent pelvic infections.
-
Emotional Impact: Chronic pain and health issues can lead to emotional and psychological stress.
Preventing Fitz-Hugh–Curtis Syndrome
Prevention focuses on reducing the risk of pelvic infections. Here are some preventive measures.
-
Safe Sex Practices: Using condoms and practicing safe sex can reduce the risk of sexually transmitted infections.
-
Regular Screenings: Regular screenings for STIs can help detect and treat infections early.
-
Prompt Treatment: Treating pelvic infections promptly can prevent them from spreading to the liver.
-
Education: Educating women about the signs and symptoms of PID can lead to earlier diagnosis and treatment.
-
Vaccinations: Vaccinations for certain infections, like HPV, can also reduce the risk of related complications.
Interesting Historical Facts
The history of FHCS provides some fascinating insights into medical advancements and the understanding of this condition.
-
First Descriptions: The syndrome was first described in the 1930s, highlighting the long-standing recognition of the condition.
-
Early Treatments: Early treatments were limited and often ineffective, underscoring the importance of modern antibiotics.
-
Medical Evolution: The understanding and treatment of FHCS have evolved significantly over the decades.
-
Research Advances: Ongoing research continues to improve the diagnosis and management of the syndrome.
-
Awareness Campaigns: Increased awareness has led to better recognition and treatment of FHCS in recent years.
Lesser-Known Facts About Fitz-Hugh–Curtis Syndrome
Here are some lesser-known but equally important facts about FHCS.
-
Rare in Men: While primarily affecting women, FHCS can occasionally occur in men.
-
Not Always Symptomatic: Some individuals may have FHCS without noticeable symptoms.
-
Global Occurrence: FHCS is found worldwide, though its prevalence varies by region.
-
Age Range: It can affect women of all ages, but is most common in those of reproductive age.
-
Misdiagnosis: Due to its rarity, FHCS is often misdiagnosed as other abdominal conditions.
Modern Research and Future Directions
Research continues to shed light on FHCS, leading to better treatments and outcomes. Here are some current research trends.
-
Genetic Factors: Studies are exploring potential genetic factors that may predispose individuals to FHCS.
-
New Antibiotics: Research into new antibiotics aims to improve treatment efficacy and reduce resistance.
-
Non-Invasive Diagnostics: Advances in imaging and diagnostic techniques are making non-invasive diagnosis more accurate.
-
Patient Education: Efforts to educate patients about FHCS are helping to improve early detection and treatment.
-
Global Collaboration: International research collaborations are enhancing the understanding and management of FHCS.
Final Thoughts on Fitz-Hugh–Curtis Syndrome
Fitz-Hugh–Curtis Syndrome, though rare, is a significant condition that links pelvic inflammatory disease to liver inflammation. Recognizing symptoms like sharp pain in the upper right abdomen and understanding the connection to PID can lead to quicker diagnosis and treatment. Early intervention often involves antibiotics, which can prevent complications and promote recovery. Awareness of this syndrome is crucial for those at risk, especially women with a history of PID. By staying informed and seeking prompt medical attention, individuals can manage symptoms effectively and reduce the risk of long-term health issues. Remember, knowledge is power when it comes to health. If you or someone you know experiences symptoms, consult a healthcare professional. Stay proactive about your health and spread awareness about Fitz-Hugh–Curtis Syndrome to help others stay informed.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
