A20 deficiency is a rare genetic disorder that affects the immune system. This condition results from mutations in the TNFAIP3 gene, which plays a crucial role in regulating inflammation. People with A20 deficiency often experience chronic inflammation, leading to various health issues such as autoimmune diseases, recurrent infections, and even cancer. Understanding this condition is vital for those affected and their families, as it can help manage symptoms and improve quality of life. In this blog post, we will explore 35 facts about A20 deficiency, shedding light on its causes, symptoms, and potential treatments. Get ready to learn more about this complex disorder and how it impacts lives.
Key Takeaways:
- A20 Deficiency is a rare genetic disorder causing chronic inflammation and autoimmune issues. Genetic testing and immunosuppressive treatments are key for managing symptoms and improving quality of life.
- Ongoing research aims to develop gene therapy and new biologics for A20 Deficiency. Patient registries and collaboration between researchers, clinicians, and patient advocacy groups are essential for advancing understanding and treatment options.
What is A20 Deficiency?
A20 deficiency is a rare genetic disorder that affects the immune system. It can lead to various health issues, including inflammation and autoimmunity. Here are some fascinating facts about this condition.
-
A20 deficiency is caused by mutations in the TNFAIP3 gene, which plays a crucial role in regulating inflammation.
-
The TNFAIP3 gene encodes the A20 protein, which helps control the body's immune response to prevent excessive inflammation.
-
A20 protein acts as a brake on the immune system, ensuring it doesn't overreact to infections or injuries.
-
Without A20, the immune system can become hyperactive, leading to chronic inflammation and tissue damage.
-
A20 deficiency is inherited in an autosomal recessive manner, meaning both parents must carry a copy of the mutated gene.
Symptoms of A20 Deficiency
The symptoms of A20 deficiency can vary widely, making it challenging to diagnose. Here are some common signs to look out for.
-
Chronic inflammation is a hallmark of A20 deficiency, often affecting multiple organs.
-
Autoimmune diseases such as lupus and rheumatoid arthritis are frequently associated with A20 deficiency.
-
Recurrent infections can occur due to the immune system's inability to regulate itself properly.
-
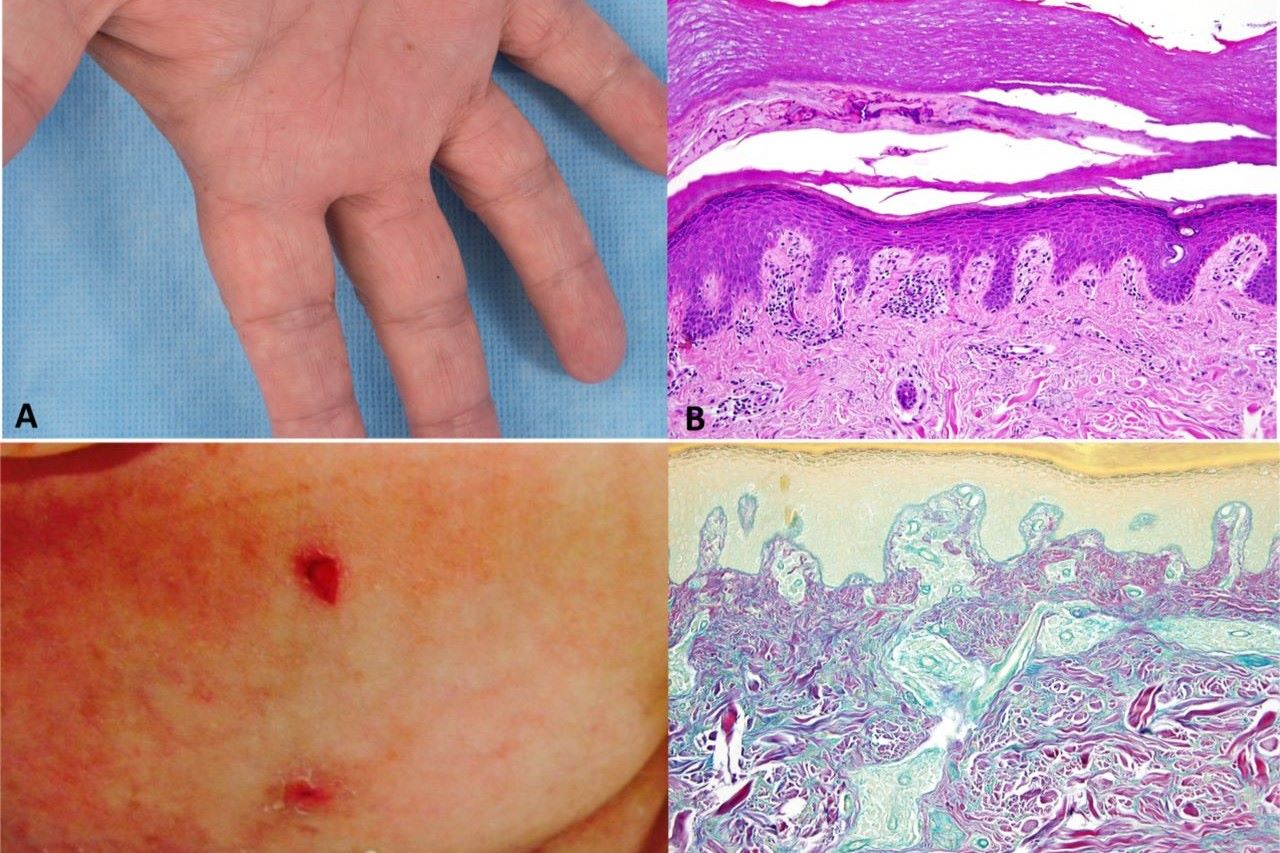
Skin rashes and lesions are common, often appearing as red, inflamed patches.
-
Gastrointestinal issues like diarrhea and abdominal pain may also be present.
Diagnosing A20 Deficiency
Diagnosing A20 deficiency involves a combination of genetic testing and clinical evaluation. Here are some key points about the diagnostic process.
-
Genetic testing is essential for confirming a diagnosis of A20 deficiency by identifying mutations in the TNFAIP3 gene.
-
Family history can provide clues, as A20 deficiency is inherited and may affect multiple family members.
-
Blood tests can reveal elevated levels of inflammatory markers, indicating an overactive immune system.
-
Biopsies of affected tissues may show signs of chronic inflammation and immune cell infiltration.
-
Clinical evaluation by a specialist, such as a rheumatologist or immunologist, is crucial for a comprehensive diagnosis.
Treatment Options for A20 Deficiency
While there is no cure for A20 deficiency, various treatments can help manage symptoms and improve quality of life. Here are some common approaches.
-
Immunosuppressive drugs can help reduce inflammation and prevent the immune system from attacking the body's tissues.
-
Biologic therapies target specific components of the immune system to control inflammation more precisely.
-
Corticosteroids are often used to quickly reduce inflammation during flare-ups.
-
Antibiotics may be necessary to treat recurrent infections resulting from an overactive immune system.
-
Lifestyle changes such as a healthy diet and regular exercise can support overall health and well-being.
Research and Future Directions
Ongoing research aims to better understand A20 deficiency and develop more effective treatments. Here are some exciting developments in the field.
-
Gene therapy holds promise for correcting the underlying genetic mutations causing A20 deficiency.
-
New biologics are being developed to target specific pathways involved in inflammation and autoimmunity.
-
Clinical trials are underway to test the safety and efficacy of novel treatments for A20 deficiency.
-
Patient registries help researchers gather data on the natural history of A20 deficiency and identify potential therapeutic targets.
-
Collaboration between researchers, clinicians, and patient advocacy groups is essential for advancing our understanding of A20 deficiency.
Living with A20 Deficiency
Managing A20 deficiency requires a multidisciplinary approach and support from healthcare professionals, family, and friends. Here are some tips for living with this condition.
-
Regular check-ups with healthcare providers are crucial for monitoring disease progression and adjusting treatment plans.
-
Support groups can provide emotional support and practical advice from others living with A20 deficiency.
-
Education about the condition helps patients and their families make informed decisions about their care.
-
Mental health care is important, as chronic illness can take a toll on emotional well-being.
-
Advocacy for research and awareness can help improve the lives of those affected by A20 deficiency.
Interesting Facts About A20 Deficiency
Here are some additional intriguing facts about A20 deficiency that highlight its complexity and the ongoing efforts to understand it better.
-
A20 deficiency was first identified in 2016, making it a relatively new area of study.
-
Animal models have been instrumental in uncovering the role of A20 in immune regulation.
-
Environmental factors such as infections and stress can trigger flare-ups in individuals with A20 deficiency.
-
Personalized medicine approaches are being explored to tailor treatments to each patient's unique genetic makeup.
-
Public awareness campaigns aim to educate the public and healthcare professionals about A20 deficiency, leading to earlier diagnosis and better outcomes.
Final Thoughts on A20 Deficiency
A20 deficiency, though rare, has significant implications for those affected. Understanding the genetic mutation behind this condition helps in diagnosing and managing symptoms more effectively. Early detection can lead to better treatment options, improving the quality of life for patients.
Research continues to uncover more about this condition, offering hope for future advancements. Staying informed and connected with medical professionals is crucial for those dealing with A20 deficiency.
By spreading awareness, we can support ongoing research and provide better resources for affected individuals. Remember, knowledge is power. The more we learn about A20 deficiency, the better equipped we are to tackle its challenges.
Stay curious, stay informed, and always advocate for your health.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
