What is a Pancreatic Islet Cell Neoplasm? It's a rare type of tumor that forms in the hormone-producing cells of the pancreas. These tumors can be benign or malignant and often affect how the body regulates blood sugar. Why should you care? Because understanding these tumors can help in early detection and treatment, which can save lives. Did you know that these neoplasms can produce hormones like insulin, glucagon, and somatostatin? This can lead to various symptoms, from low blood sugar to digestive issues. Want to know more? Stick around as we dive into 30 intriguing facts about Pancreatic Islet Cell Neoplasms.
Key Takeaways:
- Pancreatic islet cell neoplasm, also known as PNETs, are rare tumors that can produce hormones, causing specific symptoms. Early detection and treatment are crucial for better survival outcomes.
- Research and advances in medical science offer hope for improved understanding and treatment of PNETs. Ongoing studies explore immunotherapy, new imaging techniques, and genetic research for better outcomes.
What is Pancreatic Islet Cell Neoplasm?
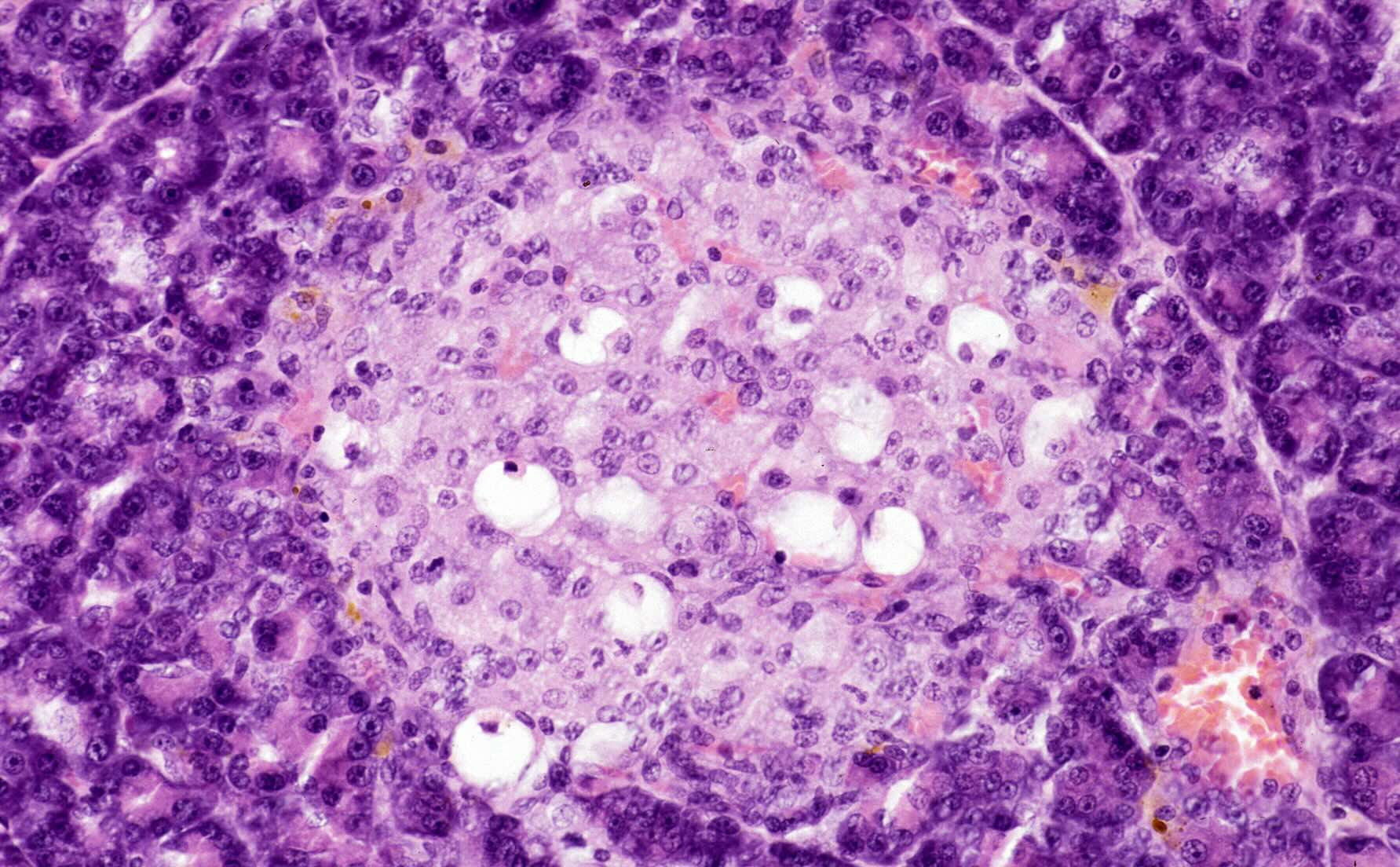
Pancreatic islet cell neoplasm, also known as pancreatic neuroendocrine tumors (PNETs), are rare tumors that arise from the hormone-producing islet cells of the pancreas. These tumors can be benign or malignant and have unique characteristics compared to other pancreatic cancers.
- Pancreatic islet cell neoplasms account for only 1-2% of all pancreatic tumors.
- They originate from the endocrine (hormone-producing) cells of the pancreas.
- PNETs can produce hormones like insulin, glucagon, and gastrin, leading to various symptoms.
- These tumors are classified into functional and non-functional types based on hormone production.
- Functional PNETs cause symptoms related to hormone overproduction, while non-functional ones often remain asymptomatic until they grow large.
Symptoms of Pancreatic Islet Cell Neoplasm
Symptoms of pancreatic islet cell neoplasm vary depending on whether the tumor is functional or non-functional. Functional tumors produce excess hormones, leading to specific symptoms.
- Insulinomas, a type of functional PNET, cause hypoglycemia due to excess insulin production.
- Gastrinomas lead to Zollinger-Ellison syndrome, characterized by severe peptic ulcers and diarrhea.
- Glucagonomas cause diabetes-like symptoms, including high blood sugar and weight loss.
- VIPomas produce vasoactive intestinal peptide, leading to chronic diarrhea and electrolyte imbalance.
- Non-functional PNETs may cause abdominal pain, jaundice, or weight loss as they grow larger.
Diagnosis of Pancreatic Islet Cell Neoplasm
Diagnosing pancreatic islet cell neoplasm involves various imaging techniques and laboratory tests to identify the tumor and its hormonal activity.
- Blood tests can detect elevated hormone levels indicative of functional PNETs.
- Imaging studies like CT scans, MRI, and PET scans help locate the tumor and assess its size.
- Endoscopic ultrasound (EUS) provides detailed images of the pancreas and allows for biopsy.
- Octreotide scans use a radioactive substance to detect neuroendocrine tumors.
- Genetic testing may be recommended for patients with a family history of PNETs or related syndromes.
Treatment Options for Pancreatic Islet Cell Neoplasm
Treatment for pancreatic islet cell neoplasm depends on the type, size, and spread of the tumor. Options range from surgery to medication and targeted therapies.
- Surgical removal is the primary treatment for localized PNETs.
- For metastatic PNETs, debulking surgery can reduce tumor burden and alleviate symptoms.
- Medications like somatostatin analogs control hormone-related symptoms in functional PNETs.
- Targeted therapies, such as everolimus and sunitinib, inhibit tumor growth.
- Chemotherapy may be used for aggressive or advanced PNETs.
Prognosis and Survival Rates
The prognosis for pancreatic islet cell neoplasm varies based on factors like tumor type, stage, and treatment response. Generally, PNETs have a better prognosis than other pancreatic cancers.
- The 5-year survival rate for localized PNETs is around 90%.
- For regional PNETs with lymph node involvement, the 5-year survival rate drops to 70%.
- Metastatic PNETs have a 5-year survival rate of approximately 30%.
- Early detection and treatment significantly improve survival outcomes.
- Functional PNETs often have a better prognosis due to earlier symptom presentation.
Research and Advances in Pancreatic Islet Cell Neoplasm
Ongoing research aims to improve the understanding, diagnosis, and treatment of pancreatic islet cell neoplasm. Advances in medical science offer hope for better outcomes.
- Immunotherapy is being explored as a potential treatment for PNETs.
- New imaging techniques, like Ga-68 DOTATATE PET/CT, provide more accurate tumor detection.
- Clinical trials are investigating novel drugs and combination therapies for PNETs.
- Genetic research helps identify hereditary syndromes associated with PNETs, aiding in early detection.
- Patient registries and databases contribute to a better understanding of PNETs and their management.
Final Thoughts on Pancreatic Islet Cell Neoplasm
Pancreatic islet cell neoplasm, though rare, holds significant importance in the medical field. Understanding its symptoms, diagnosis, and treatment options can make a world of difference for those affected. Early detection remains crucial, as it often leads to better outcomes.
Advancements in medical research continue to shed light on more effective treatments, offering hope to patients and their families. Staying informed about the latest developments and maintaining regular check-ups can help manage the condition more effectively.
Remember, knowledge is power. By staying educated about pancreatic islet cell neoplasm, you can take proactive steps toward better health. Whether you're a patient, caregiver, or just someone interested in medical facts, this information can be a valuable resource. Keep learning, stay vigilant, and always consult healthcare professionals for personalized advice.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
