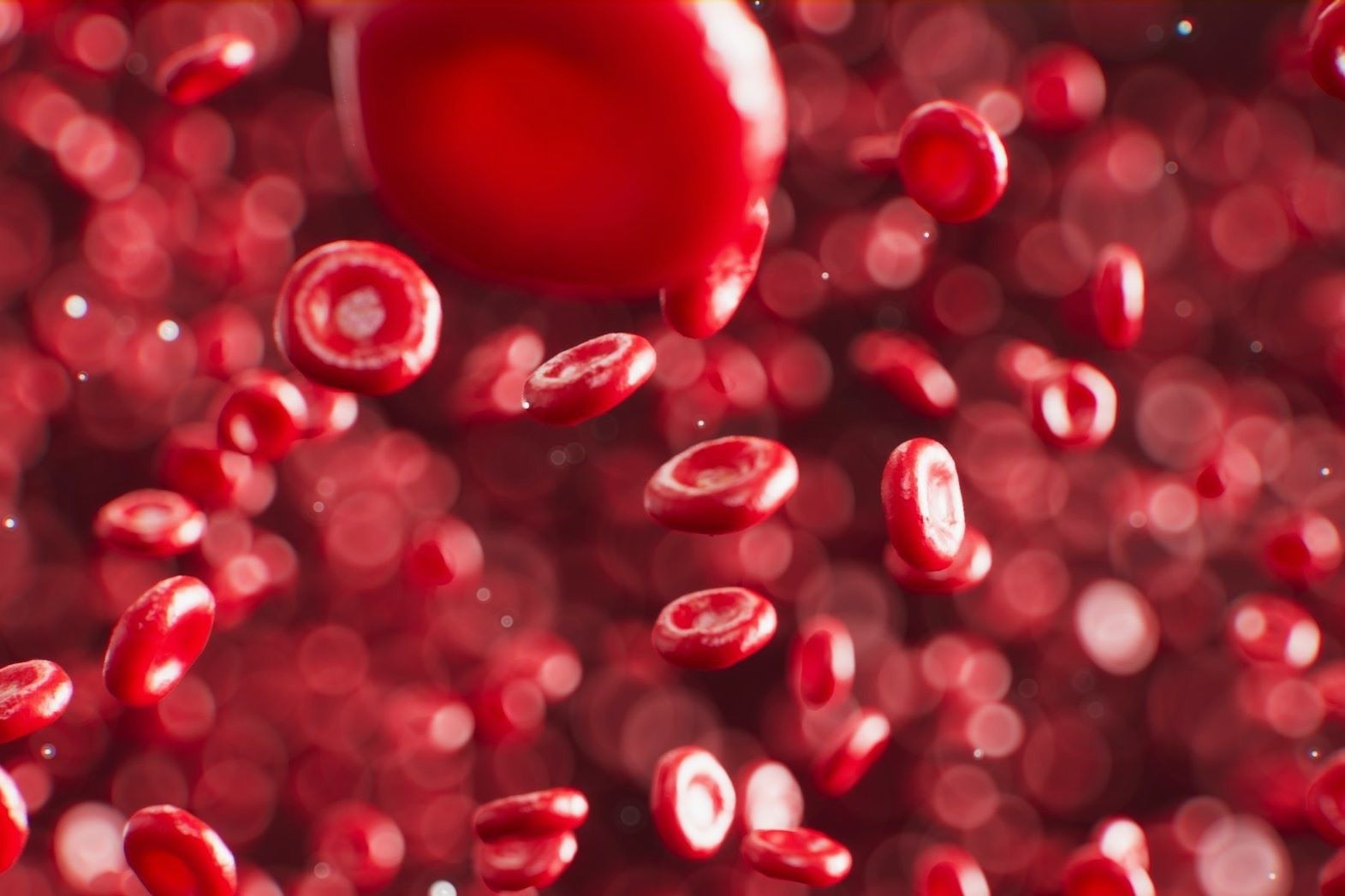
Warm-reacting-antibody hemolytic anemia is a condition where the immune system mistakenly attacks and destroys red blood cells. This type of anemia can lead to fatigue, shortness of breath, and jaundice. Warm-reacting antibodies are most active at body temperature, making them particularly troublesome. Understanding this condition involves knowing its causes, symptoms, and treatments. Autoimmune disorders, certain medications, and infections can trigger it. Diagnosing involves blood tests and sometimes bone marrow exams. Treatments range from steroids to immunosuppressive drugs. In severe cases, a splenectomy might be necessary. Living with this condition requires regular medical check-ups and lifestyle adjustments to manage symptoms effectively.
Key Takeaways:
- Warm-Reacting-Antibody Hemolytic Anemia is an autoimmune disorder where the body attacks its own red blood cells, causing symptoms like fatigue, jaundice, and dark urine. Treatment options include corticosteroids, immunosuppressants, and rituximab.
- Ongoing research is exploring new therapies for Warm-Reacting-Antibody Hemolytic Anemia, aiming to improve treatment effectiveness and quality of life for patients.
What is Warm-Reacting-Antibody Hemolytic Anemia?
Warm-reacting-antibody hemolytic anemia (WAIHA) is a type of autoimmune disorder where the body's immune system mistakenly attacks its own red blood cells. This condition can lead to various symptoms and complications. Let's dive into some intriguing facts about WAIHA.
Causes and Mechanisms
Understanding the root causes and mechanisms of WAIHA can help in managing the condition better.
- Autoimmune Disorder: WAIHA is an autoimmune disorder where the immune system produces antibodies that attack red blood cells.
- Warm Antibodies: The antibodies involved in WAIHA react optimally at body temperature (37°C or 98.6°F).
- IgG Antibodies: The primary antibodies responsible for WAIHA are of the IgG type.
- Spleen Involvement: The spleen plays a significant role in the destruction of antibody-coated red blood cells.
- Secondary Causes: WAIHA can be secondary to other conditions like lupus, lymphoma, or certain infections.
- Drug-Induced: Some medications, such as penicillin, can trigger WAIHA.
Symptoms and Diagnosis
Recognizing the symptoms and understanding the diagnostic process is crucial for early intervention.
- Fatigue: One of the most common symptoms is extreme fatigue due to reduced oxygen-carrying capacity.
- Jaundice: Yellowing of the skin and eyes occurs because of increased bilirubin levels from red blood cell breakdown.
- Dark Urine: Hemoglobin released from destroyed red blood cells can cause dark-colored urine.
- Pallor: Pale skin is another symptom due to decreased red blood cell count.
- Splenomegaly: Enlargement of the spleen can occur as it works harder to remove damaged cells.
- Blood Tests: Diagnosis often involves blood tests showing anemia, increased reticulocyte count, and positive direct antiglobulin test (DAT).
Treatment Options
Various treatment options are available to manage WAIHA effectively.
- Corticosteroids: The first line of treatment usually involves corticosteroids like prednisone to suppress the immune system.
- Immunosuppressants: Drugs like azathioprine or cyclophosphamide may be used if corticosteroids are ineffective.
- Rituximab: This monoclonal antibody targets B cells and can be effective in treating WAIHA.
- Splenectomy: Surgical removal of the spleen may be considered in severe cases.
- Blood Transfusions: In cases of severe anemia, blood transfusions may be necessary.
- Folic Acid: Supplementing with folic acid helps in the production of new red blood cells.
Prognosis and Complications
Knowing the potential outcomes and complications can help in preparing for long-term management.
- Chronic Condition: WAIHA can be a chronic condition requiring long-term treatment and monitoring.
- Relapses: Patients may experience relapses, especially if the underlying cause is not addressed.
- Infections: Immunosuppressive treatments can increase the risk of infections.
- Thrombosis: There is an increased risk of blood clots due to the hypercoagulable state.
- Organ Damage: Severe anemia can lead to damage in organs like the heart and kidneys.
- Quality of Life: Managing symptoms and treatment side effects is crucial for maintaining a good quality of life.
Research and Future Directions
Ongoing research aims to improve the understanding and treatment of WAIHA.
- New Therapies: Researchers are exploring new therapies, including targeted biological agents, to treat WAIHA more effectively.
Final Thoughts on Warm-Reacting-Antibody Hemolytic Anemia
Warm-reacting-antibody hemolytic anemia (WAIHA) is a complex condition where the immune system mistakenly attacks red blood cells. This leads to symptoms like fatigue, jaundice, and shortness of breath. Understanding the causes, symptoms, and treatments can help manage this condition better. Treatments often include steroids, immunosuppressants, or even blood transfusions. Early diagnosis and proper medical care are crucial for improving quality of life.
Staying informed about WAIHA can make a big difference. Whether you're a patient, caregiver, or just curious, knowing these facts can help you navigate the challenges that come with this condition. Always consult healthcare professionals for personalized advice and treatment plans. Knowledge is power, and being well-informed can lead to better health outcomes.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.


