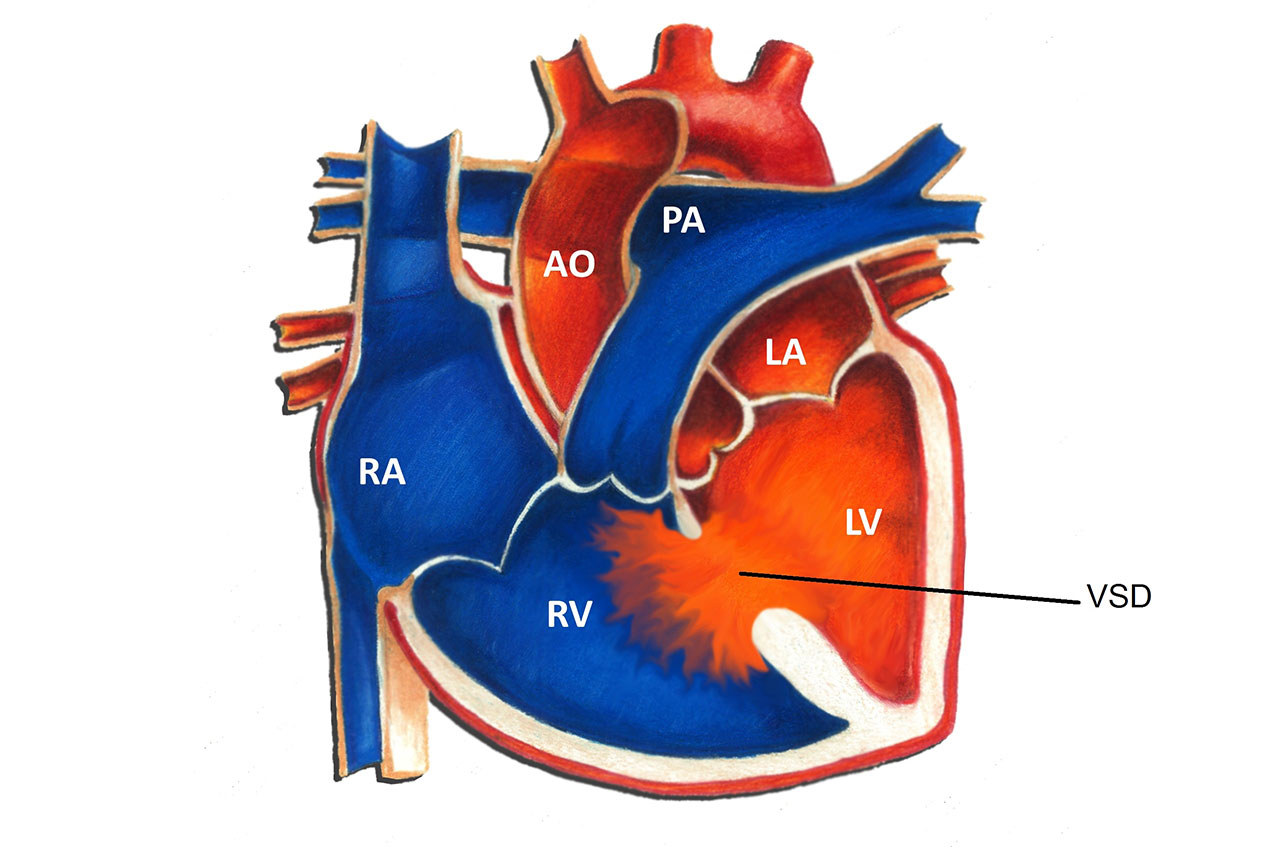
What is a Ventricular Septal Defect (VSD)? It's a heart condition where a hole exists in the wall separating the heart's lower chambers, known as ventricles. This defect allows blood to mix between the left and right ventricles, which can lead to increased blood flow to the lungs and heart. VSDs are among the most common congenital heart defects, often detected in infants. Some small VSDs may close on their own, while larger ones might require surgical intervention to prevent complications. Symptoms can include shortness of breath, rapid breathing, or poor weight gain in babies. Understanding VSDs is crucial for early diagnosis and effective management. Whether you're a parent, student, or just curious, learning about VSDs helps in recognizing signs and seeking timely medical advice.
Key Takeaways:
- Ventricular Septal Defect (VSD) is the most common congenital heart defect, affecting 1 in every 500 live births. Small VSDs may close on their own, while larger ones may require surgery.
- Early detection of VSD through prenatal ultrasound and echocardiogram can lead to better management and outcomes. Living with VSD requires regular check-ups, heart-healthy habits, and emotional support.
Understanding Ventricular Septal Defect
Ventricular Septal Defect (VSD) is a heart condition that affects many people worldwide. It involves a hole in the wall separating the heart's lower chambers. Let's explore some interesting facts about this condition.
-
Common Congenital Heart Defect: VSD is the most common congenital heart defect, occurring in about 1 in every 500 live births.
-
Size Matters: The size of the defect can vary greatly, from tiny pinholes to large openings.
-
Location Variability: VSDs can occur in different parts of the septum, including the muscular and membranous sections.
-
Symptoms Depend on Size: Small VSDs may cause no symptoms, while larger ones can lead to heart failure or other complications.
-
Spontaneous Closure: Many small VSDs close on their own during childhood without medical intervention.
Causes and Risk Factors
Understanding what causes VSD can help in managing and preventing it. Here are some key points to consider.
-
Genetic Factors: Some VSDs are linked to genetic syndromes, such as Down syndrome.
-
Environmental Influences: Maternal exposure to certain substances during pregnancy can increase the risk of VSD.
-
Family History: A family history of heart defects can raise the likelihood of VSD in newborns.
-
Maternal Health: Conditions like diabetes in the mother can contribute to the development of VSD.
-
Unknown Causes: In many cases, the exact cause of VSD remains unidentified.
Diagnosis and Detection
Detecting VSD early can lead to better management and outcomes. Here's how it's typically diagnosed.
-
Prenatal Ultrasound: VSD can sometimes be detected before birth through a detailed ultrasound.
-
Echocardiogram: This is the most common test used to diagnose VSD after birth.
-
Chest X-ray: Can show signs of heart enlargement or fluid in the lungs.
-
Electrocardiogram (ECG): Helps assess the heart's electrical activity and detect any abnormalities.
-
Cardiac MRI: Provides detailed images of the heart's structure, useful for complex cases.
Treatment Options
Treatment for VSD varies based on the defect's size and symptoms. Here are some common approaches.
-
Watchful Waiting: Small VSDs that aren't causing symptoms may just be monitored over time.
-
Medications: Drugs can help manage symptoms like heart failure or high blood pressure.
-
Surgical Repair: Larger VSDs often require surgery to close the hole.
-
Catheter Procedure: A less invasive option where a device is used to close the VSD via a catheter.
-
Lifestyle Adjustments: Regular follow-ups and a heart-healthy lifestyle are crucial for managing VSD.
Potential Complications
While many with VSD live healthy lives, complications can arise. Here are some to be aware of.
-
Heart Failure: Large VSDs can lead to heart failure if untreated.
-
Pulmonary Hypertension: Increased blood flow to the lungs can cause high blood pressure in the lung arteries.
-
Endocarditis: A risk of infection in the heart lining, especially in those with larger defects.
-
Arrhythmias: Irregular heartbeats can occur due to changes in heart structure.
-
Growth Delays: Some children with VSD may experience slower growth and development.
Living with VSD
Living with VSD requires some adjustments, but many lead normal lives. Here are some insights.
-
Regular Check-ups: Ongoing medical care is essential to monitor heart health.
-
Exercise Considerations: Most can participate in regular activities, but some may need to avoid strenuous sports.
-
Dietary Needs: A balanced diet supports overall heart health.
-
Emotional Support: Counseling or support groups can help families cope with the condition.
-
Education and Awareness: Understanding VSD helps in managing it effectively.
VSD in Adults
While often diagnosed in childhood, VSD can persist into adulthood. Here's what to know.
-
Late Diagnosis: Some adults are diagnosed with VSD later in life, often due to mild symptoms.
-
Surgical History: Adults who had VSD repair as children may need follow-up surgeries.
-
Pregnancy Considerations: Women with VSD should consult doctors before pregnancy for risk assessment.
-
Lifestyle Modifications: Heart-healthy habits remain crucial throughout life.
-
Regular Monitoring: Adult VSD patients need lifelong cardiac care.
Research and Advances
Ongoing research continues to improve VSD treatment and understanding. Here are some recent developments.
-
Genetic Studies: Research is exploring the genetic basis of VSD to improve diagnosis and treatment.
-
Innovative Surgeries: New surgical techniques are making repairs safer and more effective.
-
Non-invasive Treatments: Advances in catheter-based procedures offer less invasive options.
-
Long-term Outcomes: Studies are focusing on the long-term health of those with VSD.
-
Global Awareness: Efforts are underway to raise awareness and improve care worldwide.
Famous Cases
Some well-known individuals have lived with VSD, bringing attention to the condition.
-
Celebrity Advocacy: Some celebrities have shared their VSD experiences to raise awareness.
-
Historical Figures: Historical records suggest some famous figures may have had VSD.
-
Athletes with VSD: Several athletes have achieved success despite having VSD.
-
Public Figures: Politicians and public figures have spoken about their VSD journeys.
-
Inspirational Stories: Many individuals with VSD have inspiring stories of overcoming challenges.
Myths and Misconceptions
Misunderstandings about VSD can lead to confusion. Let's clear up some common myths.
-
Myth: VSD Always Requires Surgery: Not all VSDs need surgical intervention.
-
Myth: VSD is Rare: It's actually the most common congenital heart defect.
-
Myth: VSD Prevents Normal Life: Many with VSD live full, active lives.
-
Myth: Only Children Have VSD: Adults can have VSD too, either undiagnosed or persistent from childhood.
-
Myth: VSD is Always Genetic: While genetics play a role, many cases have no known cause.
Understanding Ventricular Septal Defect
Ventricular Septal Defect (VSD) is a heart condition that affects many people worldwide. Knowing the symptoms, causes, and treatment options can make a big difference in managing this condition. VSD occurs when there's a hole in the wall separating the heart's lower chambers. This can lead to heart murmurs, fatigue, and breathing difficulties. While some VSDs close on their own, others might need medical intervention. Treatments range from medications to surgical procedures. Early detection is crucial for effective management. Regular check-ups with a healthcare provider can help monitor heart health and catch any issues early. For those living with VSD, understanding the condition and maintaining a healthy lifestyle can improve quality of life. Stay informed, ask questions, and work closely with healthcare professionals to ensure the best care possible. Knowledge empowers individuals and families dealing with VSD.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
