Sepsis is a life-threatening condition where the body's response to infection causes widespread inflammation, leading to organ failure and death. Affecting millions globally each year, it claims at least 11 million lives annually. Recognizing sepsis early is crucial, as symptoms like fever, confusion, and difficulty breathing can escalate quickly. Children under 5 and older adults are particularly vulnerable. Preventive measures, such as good hygiene and timely treatment of infections, are essential. Understanding sepsis—its causes, symptoms, and treatments—can save lives. This article dives into 50 key facts about sepsis to raise awareness and promote early intervention.
Key Takeaways:
- Sepsis is a serious condition that affects millions worldwide, with 1 in 5 deaths linked to sepsis. Early recognition of symptoms and preventive measures are crucial in saving lives.
- Understanding the causes, symptoms, and long-term effects of sepsis is essential for early diagnosis and effective treatment. Public awareness and innovative technologies play a key role in improving sepsis outcomes.
Understanding Sepsis
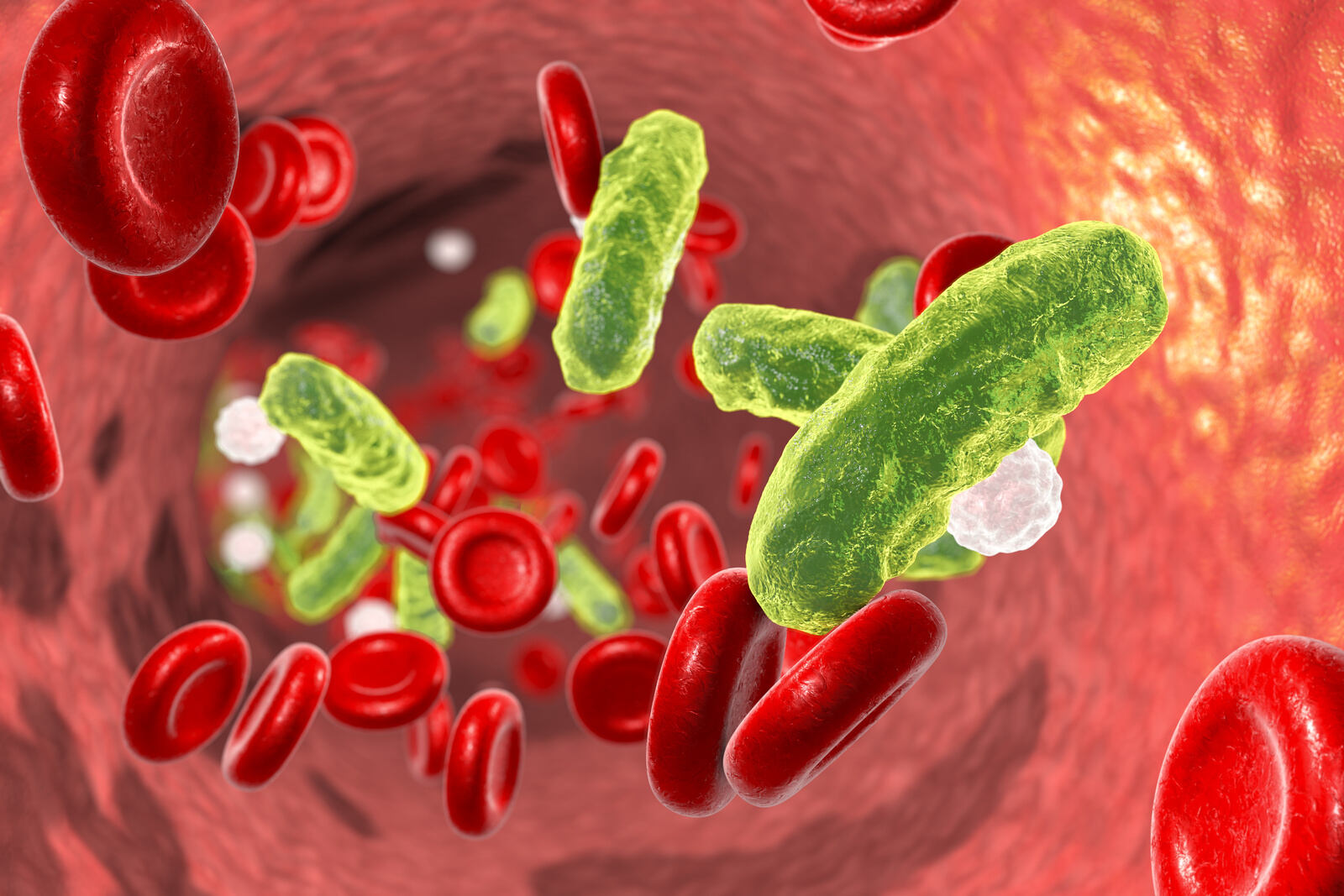
Sepsis is a critical medical condition that demands immediate attention. It occurs when the body's immune system overreacts to an infection, leading to widespread inflammation and organ dysfunction. Here are some essential facts to help you understand sepsis better.
-
Definition of Sepsis: Sepsis is a systemic inflammatory response to an infectious process that can lead to end-stage organ dysfunction and death.
-
Global Prevalence: Sepsis affects approximately 47 to 50 million people worldwide each year, with at least 11 million deaths annually.
-
Mortality Rate: One in five deaths worldwide is associated with sepsis, making it a significant cause of mortality globally.
-
Age Distribution: 40% of sepsis cases occur in children under the age of 5.
-
Hospital Readmissions: Sepsis is the number one cause of hospital readmissions, highlighting the need for effective management and prevention strategies.
Causes and Risk Factors
Understanding what causes sepsis and who is at risk can help in early detection and prevention.
-
Causes of Sepsis: Sepsis is always caused by an infection, which can be bacterial, viral, fungal, or noninfectious in nature. Common sources include pneumonia, intra-abdominal infections, endovascular infections, and urinary tract infections.
-
Hospital-Acquired Infections: 80% of sepsis cases occur outside of a hospital setting, but hospital-acquired infections are a significant concern, especially in lower-middle-income countries (LMICs).
-
Risk Factors: People who are older, very young, pregnant, or have other health problems are at higher risk for developing sepsis.
Recognizing Symptoms
Early recognition of sepsis symptoms can save lives. Knowing what to look for is crucial.
-
Symptoms: Common signs and symptoms of sepsis include fever or low temperature, confusion, difficulty breathing, clammy and sweaty skin, extreme body pain or discomfort, high heart rate, weak pulse or low blood pressure, and low urine output.
-
Symptoms in Children: In children, symptoms can include fast breathing, convulsions, pale skin, lethargy, difficulty waking up, and feeling cold to the touch. Children under 5 may also experience difficulty feeding, frequent vomiting, or lack of urination.
-
Early Recognition: Sepsis is a medical emergency that requires immediate recognition and treatment. Early diagnosis is crucial to improve outcomes.
Pathophysiology and Organ Dysfunction
Understanding how sepsis affects the body can help in managing and treating it effectively.
-
Pathophysiology: The body's reaction to sepsis involves an extreme immune response, leading to widespread inflammation, blood clots, and leaky blood vessels. This can impair blood flow to organs, causing damage and dysfunction.
-
Organ Dysfunction: Sepsis can lead to multiple organ failure, including the lungs, kidneys, and liver, which can result in septic shock and death if not treated promptly.
Prevention and Early Treatment
Preventing sepsis and treating it early can significantly improve outcomes.
-
Antimicrobial Resistance: Antimicrobial resistance is a major factor in sepsis management. Patients with resistant pathogens have a higher risk of hospital mortality and more challenging treatment outcomes.
-
Preventive Measures: Preventing sepsis involves treating infections early and practicing good hygiene at home and in healthcare settings. This includes washing hands, preparing food safely, avoiding unclean water or unsanitary toilets, getting recommended vaccines, eating a healthy diet, and breastfeeding newborns.
-
Infection Prevention: Hospitals and clinics should follow effective rules for infection prevention and control. Antibiotics should be used appropriately to treat infections, and antimicrobial stewardship programs are essential to reduce resistance.
-
Early Goal-Directed Therapy: Early goal-directed therapy (EGDT) is a revolutionary approach in managing sepsis. It involves early identification of at-risk patients, prompt treatment with antibiotics, hemodynamic optimization, and appropriate supportive care. This has significantly contributed to improved outcomes in sepsis.
Diagnostic Criteria and Challenges
Diagnosing sepsis accurately and promptly is vital for effective treatment.
-
Biomarkers: Investigations into clinically relevant biomarkers of sepsis are ongoing but have yet to yield effective results. Biomarkers could help in early diagnosis and monitoring of sepsis.
-
Sepsis-3 Criteria: The Sepsis-3 criteria define sepsis as infection with a concurrent rise in Sequential Organ Failure Assessment (SOFA) score by 2 or more points from the preinfection baseline. Cases are further classified as possible, probable, or definite based on the probability of infection and presence of other causes of organ dysfunction.
-
Hospital-Onset Sepsis: Hospital-onset sepsis is defined as sepsis arising from an infection acquired more than 48 hours after admission. Sepsis arising 48 hours or less from admission is considered present on admission.
Mortality and Preventability
Understanding the causes of sepsis-related deaths can help in developing better prevention strategies.
-
Immediate vs. Underlying Causes of Death: In hospital settings, sepsis is often the immediate cause of death, but underlying causes such as severe chronic comorbidities are more common. Most sepsis-associated deaths are unlikely to be preventable through better hospital-based care.
-
Preventability of Sepsis-Associated Deaths: Only 3.7% of sepsis-associated deaths were judged definitely or moderately preventable, highlighting the complexity of sepsis management and the need for comprehensive care strategies.
-
Common Causes of Sepsis-Associated Deaths: Among patients with sepsis as the immediate cause of death, the most common causes include pneumonia (50.5%), intra-abdominal infections (19.2%), endovascular infections (12.6%), urinary tract infections (9.6%), and unknown infectious sources (5.6%).
-
Chronic Comorbidities: The most common underlying causes of death in patients with sepsis include solid cancer, chronic heart disease, hematologic cancer, dementia, and chronic lung disease.
-
Hospice-Qualifying Conditions: Hospice-qualifying conditions were present on admission in 40.3% of sepsis-associated deaths, most commonly end-stage cancer.
-
Suboptimal Care: Suboptimal care, such as delays in antibiotics, was identified in 22.7% of sepsis-associated deaths, indicating areas for improvement in hospital care practices.
Long-Term Effects and Innovations
Surviving sepsis is just the beginning; long-term effects and new technologies play a crucial role in ongoing care.
-
Long-Term Effects: Up to 50% of sepsis survivors suffer from long-term physical and/or psychological effects, emphasizing the need for comprehensive post-acute care.
-
AI-Based Diagnosis: The National Institute of General Medical Sciences (NIGMS) funded the inception of the first FDA-approved AI-based sepsis diagnosis algorithm, the Sepsis ImmunoScore. The impact of this development on sepsis care is yet to be fully tested in real-world settings.
-
CDC Guidelines: More information about the symptoms, diagnosis, and treatment of sepsis is available from the Centers for Disease Control and Prevention (CDC).
Global Impact and Disparities
Sepsis affects people worldwide, but its impact varies significantly across different regions.
-
Global Burden: The global epidemiological burden of sepsis is difficult to ascertain, but it is estimated that more than 30 million people are affected by sepsis every year, resulting in potentially 6 million deaths annually.
-
Regional Disparities: Significant regional disparities in incidence and mortality exist, with the highest rates in lower-middle-income countries (LMICs).
-
Healthcare-Associated Infections: Healthcare-associated infections are a major concern, as they can lead to sepsis and septic shock. These infections are often caused by pathogens that are resistant to drugs, complicating treatment.
-
Antimicrobial Resistance: Antimicrobial resistance is a major factor determining clinical unresponsiveness to treatment and rapid evolution to sepsis and septic shock. It is estimated that 1.27 million deaths in 2019 were directly attributable to antimicrobial resistance.
Preventive Measures and Early Diagnosis
Preventing sepsis and diagnosing it early can save lives and reduce healthcare costs.
-
Preventive Measures in Healthcare Settings: Hospitals and clinics should implement effective infection prevention and control measures, including good hygiene practices, vaccination programs, improved sanitation, and water quality. Antibiotics should be used appropriately to treat infections.
-
Early Diagnosis and Treatment: Early diagnosis and timely and appropriate clinical management of sepsis are crucial to increase the likelihood of survival. This includes optimal antimicrobial use and fluid resuscitation.
-
Multidisciplinary Approach: Sepsis requires a multidisciplinary approach involving healthcare workers, nurses, and other medical professionals to ensure comprehensive care and improve outcomes.
Special Populations
Certain groups are more vulnerable to sepsis and require special attention.
-
Sepsis in Children: Children under 5 years old are disproportionately affected by sepsis, with almost half of all estimated sepsis cases occurring in this age group. Symptoms in children include fast breathing, convulsions, pale skin, lethargy, and difficulty waking up.
-
Sepsis in Older Adults: Older adults are also at higher risk for developing sepsis due to age-related immune system decline and comorbidities. Early recognition and treatment are critical in this population.
-
Pregnancy and Sepsis: Pregnant women are at higher risk for developing sepsis due to changes in the immune system during pregnancy. Prompt treatment is essential to prevent maternal and fetal complications.
Common Infections and Challenges in LMICs
Certain infections are more likely to lead to sepsis, and LMICs face unique challenges in managing this condition.
-
Common Infections Leading to Sepsis: Common infections that can lead to sepsis include pneumonia, intra-abdominal infections, endovascular infections, urinary tract infections, and other types of infections.
-
Sepsis in Low-Middle-Income Countries (LMICs): LMICs face significant challenges in managing sepsis due to limited resources, inadequate healthcare infrastructure, and high rates of antimicrobial resistance. Preventive measures such as good hygiene practices and vaccination programs are crucial in these settings.
Impact on Healthcare Systems
Sepsis places a significant burden on healthcare systems worldwide, necessitating effective management strategies.
-
Impact on Healthcare Systems: Sepsis places a significant burden on healthcare systems worldwide, accounting for substantial hospital costs and resource utilization. Effective management strategies are essential to reduce this burden.
-
Role of Biomarkers: Biomarkers such as C-reactive protein (CRP) and procalcitonin (PCT) are used to diagnose sepsis. However, their utility is limited by variability in levels and the need for further research to improve their specificity and sensitivity.
-
Sepsis-Related Morbidity: Sepsis survivors often experience long-term morbidity requiring ongoing treatment and support. This includes physical disabilities, psychological trauma, and potential long-term organ damage.
Innovations and Public Awareness
New technologies and public education are key to improving sepsis outcomes.
-
AI in Sepsis Management: Artificial intelligence (AI) is being explored for its potential in sepsis diagnosis and management. The Sepsis ImmunoScore is an example of AI-based diagnosis that could improve early detection and treatment.
-
CDC Recommendations: The CDC provides guidelines for the diagnosis, treatment, and prevention of sepsis. These recommendations include early recognition of symptoms, appropriate use of antimicrobials, and supportive care measures.
-
Global Awareness: World Sepsis Day on September 13th raises awareness about sepsis globally. It aims to educate the public about the risks and symptoms of sepsis and promote early recognition and treatment.
-
Research and Development: Ongoing research focuses on developing new diagnostic tools, treatments, and preventive measures for sepsis. This includes investigations into biomarkers, AI algorithms, and innovative therapeutic strategies.
-
Public Education: Public education is crucial in reducing the incidence of sepsis. Awareness campaigns should focus on recognizing symptoms early, practicing good hygiene, and seeking medical care promptly if symptoms arise.
-
Long-Term Effects: Up to 50% of sepsis survivors suffer from long-term physical and/or psychological effects, emphasizing the need for comprehensive post-acute care.
Final Thoughts on Sepsis
Sepsis is a serious condition that demands immediate attention. Affecting millions globally, it can lead to organ failure and death if not treated promptly. Recognizing symptoms like fever, confusion, and difficulty breathing is crucial. Early intervention with antibiotics and supportive care can save lives. Preventive measures, such as good hygiene and vaccinations, play a key role in reducing sepsis cases. High-risk groups include children under 5, older adults, and pregnant women. Hospitals must follow strict infection control practices to prevent hospital-acquired infections. Long-term effects can impact survivors, necessitating ongoing care. Awareness and education about sepsis are vital for early detection and treatment. By understanding its causes, symptoms, and prevention strategies, we can reduce its global burden and improve outcomes for those affected. Stay informed, practice good hygiene, and seek medical help if you suspect sepsis.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
