Reperfusion injury occurs when blood supply returns to tissue after a period of ischemia or lack of oxygen. This paradoxical damage can be more harmful than the initial lack of blood flow. Why does reperfusion injury happen? When oxygen rushes back into the tissues, it can create reactive oxygen species (ROS), leading to inflammation and cell death. This condition is common in heart attacks, strokes, and organ transplants. Understanding the mechanisms behind reperfusion injury is crucial for developing treatments to minimize damage. In this post, we will explore 50 fascinating facts about reperfusion injury, shedding light on its causes, effects, and potential therapies.
Key Takeaways:
- Reperfusion injury occurs when oxygen-starved tissues are suddenly flooded with blood, causing damage. It affects the heart, brain, and other organs, complicating treatment and organ transplantation.
- Understanding the causes and effects of reperfusion injury is crucial for developing treatments and prevention strategies. Lifestyle changes, pharmacological agents, and innovative research offer hope for minimizing its impact.
What is Reperfusion Injury?
Reperfusion injury happens when blood supply returns to tissue after a period of ischemia or lack of oxygen. This sudden restoration can cause damage rather than healing. Let's dive into some fascinating facts about this complex medical phenomenon.
- Reperfusion injury often occurs after heart attacks or strokes when blood flow is restored to the affected area.
- The damage results from oxidative stress, inflammation, and calcium overload in cells.
- It can affect various organs, including the heart, brain, kidneys, and liver.
- The term "ischemia-reperfusion injury" is often used interchangeably with reperfusion injury.
- Reperfusion injury can lead to cell death, tissue damage, and organ dysfunction.
Causes and Mechanisms
Understanding the causes and mechanisms behind reperfusion injury helps in developing treatments. Here are some key points:
- Reactive oxygen species (ROS) play a significant role in causing damage during reperfusion.
- Inflammation is another major contributor, as immune cells flood the area and release harmful substances.
- Calcium overload in cells can lead to mitochondrial dysfunction and cell death.
- Nitric oxide, while generally protective, can form harmful compounds during reperfusion.
- The sudden change in pH levels can also contribute to cellular damage.
Effects on the Heart
The heart is particularly vulnerable to reperfusion injury. Here are some specific effects:
- Myocardial stunning, a temporary loss of heart function, can occur.
- Reperfusion arrhythmias, irregular heartbeats, are common during the early stages of reperfusion.
- Microvascular obstruction, where small blood vessels remain blocked, can happen.
- The "no-reflow" phenomenon, where blood fails to reach certain areas, is a risk.
- Infarct size, the area of dead tissue, can increase due to reperfusion injury.
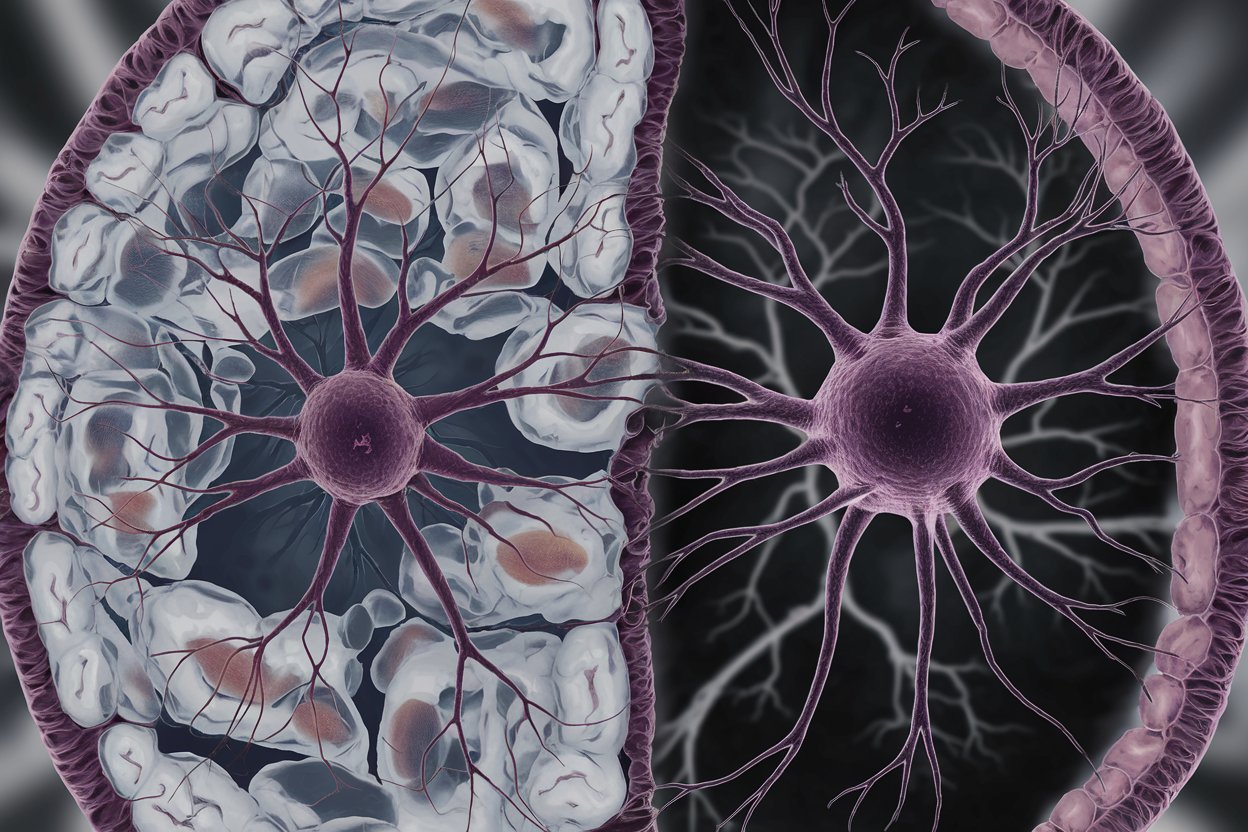
Effects on the Brain
The brain is another organ highly susceptible to reperfusion injury. Here’s how it affects the brain:
- Cerebral edema, or brain swelling, can occur.
- Blood-brain barrier disruption can lead to further complications.
- Neuronal death is a significant risk, leading to loss of brain function.
- Cognitive deficits and memory loss can result from brain reperfusion injury.
- Increased intracranial pressure is another potential outcome.
Diagnostic Methods
Identifying reperfusion injury early is crucial for effective treatment. Here are some diagnostic methods:
- Imaging techniques like MRI and CT scans can detect tissue damage.
- Blood tests can measure biomarkers indicating oxidative stress and inflammation.
- Electrocardiograms (ECGs) help identify heart-related reperfusion injury.
- Neurological assessments are used for brain reperfusion injury.
- Biopsies can provide detailed information about cellular damage.
Treatment Options
Various treatments aim to minimize reperfusion injury. Here are some approaches:
- Antioxidants can help neutralize reactive oxygen species.
- Anti-inflammatory drugs reduce inflammation and immune response.
- Calcium channel blockers prevent calcium overload in cells.
- Controlled reperfusion, gradually restoring blood flow, can minimize damage.
- Hypothermia, cooling the affected area, can reduce metabolic demand and injury.
Research and Future Directions
Ongoing research aims to better understand and treat reperfusion injury. Here are some exciting developments:
- Gene therapy is being explored to protect cells from reperfusion damage.
- Stem cell therapy shows promise in repairing damaged tissues.
- New drugs targeting specific pathways involved in reperfusion injury are in development.
- Improved imaging techniques are helping to detect and monitor injury more accurately.
- Personalized medicine approaches are being investigated to tailor treatments to individual patients.
Interesting Facts
Here are some lesser-known but intriguing facts about reperfusion injury:
- Reperfusion injury was first described in the 1960s.
- It is a significant concern in organ transplantation, affecting graft survival.
- Some animals, like certain fish and amphibians, are naturally resistant to reperfusion injury.
- Exercise preconditioning, regular physical activity, can reduce the risk of reperfusion injury.
- Certain foods rich in antioxidants, like berries and nuts, may offer some protection.
Clinical Implications
Reperfusion injury has significant clinical implications. Here’s why it matters:
- It complicates the treatment of heart attacks and strokes.
- Managing reperfusion injury can improve outcomes in organ transplantation.
- Understanding reperfusion injury helps in developing better surgical techniques.
- It influences the design of medical devices, like stents and catheters.
- Reperfusion injury research contributes to broader knowledge about cell death and survival.
Prevention Strategies
Preventing reperfusion injury is a key focus for researchers and clinicians. Here are some strategies:
- Preconditioning, exposing tissues to short periods of ischemia, can build resistance.
- Postconditioning, applying brief interruptions during reperfusion, can reduce damage.
- Pharmacological agents are being developed to protect tissues during reperfusion.
- Lifestyle changes, like a healthy diet and regular exercise, can lower the risk.
- Early intervention and rapid treatment of ischemic events are crucial for prevention.
Final Thoughts on Reperfusion Injury
Reperfusion injury is a complex process that occurs when blood supply returns to tissue after a period of ischemia or lack of oxygen. This paradoxical damage can lead to inflammation, oxidative stress, and even cell death. Understanding the mechanisms behind reperfusion injury is crucial for developing effective treatments. Researchers are exploring various strategies, including antioxidants, anti-inflammatory agents, and controlled reperfusion techniques, to mitigate this damage. While significant progress has been made, more research is needed to fully understand and combat reperfusion injury. Staying informed about the latest advancements can help healthcare professionals better manage conditions like heart attacks and strokes. By continuing to study and address this issue, we can improve patient outcomes and reduce the long-term effects of ischemic events.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
