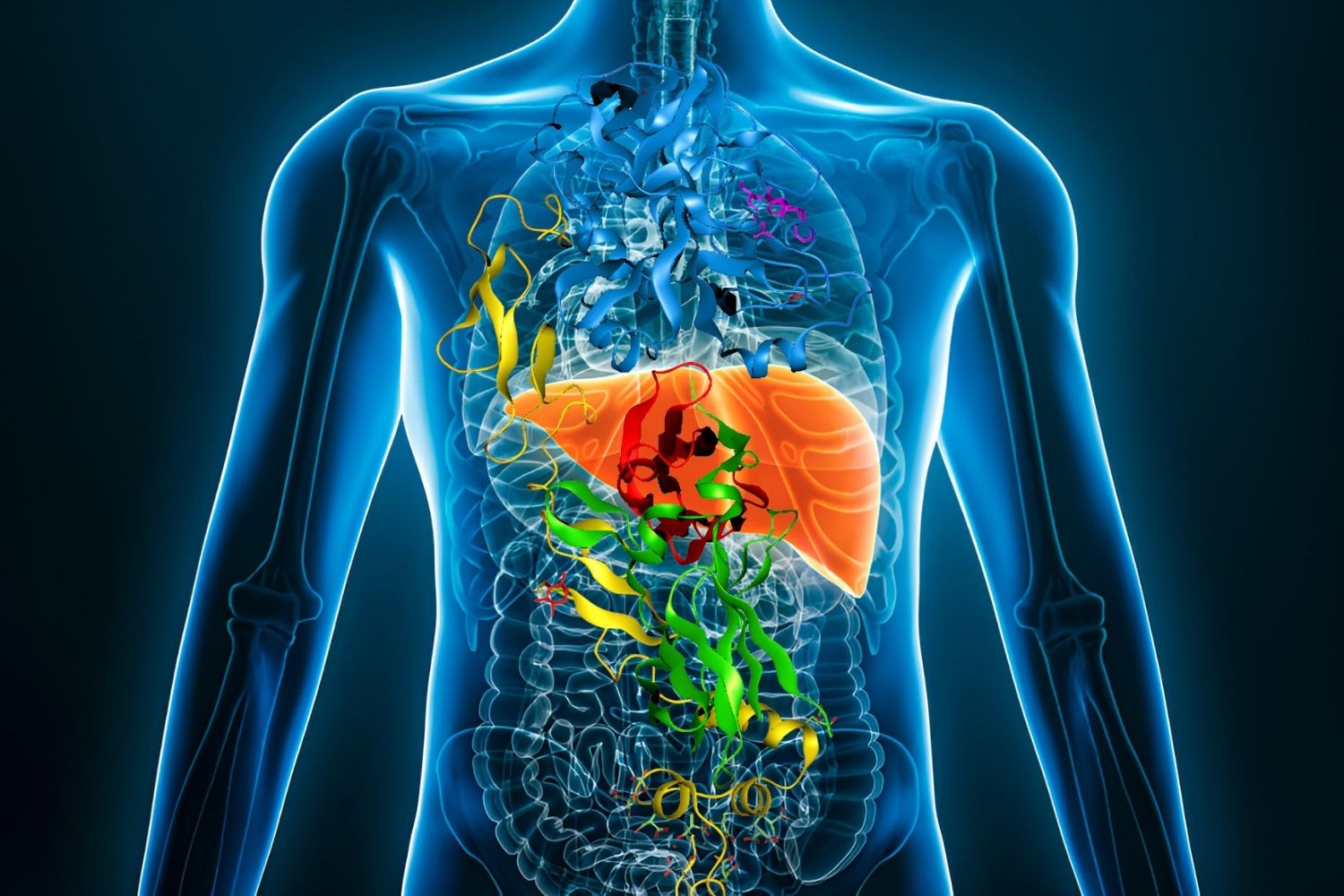
Primary Sclerosing Cholangitis (PSC) is a rare, chronic liver disease that affects the bile ducts. PSC causes inflammation and scarring of these ducts, leading to liver damage over time. While the exact cause remains unknown, it often occurs alongside other autoimmune diseases like ulcerative colitis. Symptoms can include fatigue, itching, and jaundice, but some people may not show signs until the disease has progressed. PSC can lead to serious complications, including liver failure and bile duct cancer. Understanding this condition is crucial for managing its impact on daily life. Here are 50 facts to help you grasp the essentials of Primary Sclerosing Cholangitis.
Key Takeaways:
- Primary Sclerosing Cholangitis is a rare liver disease that can cause serious damage over time. It's important to recognize symptoms early and seek regular medical care to manage the condition effectively.
- Patients with Primary Sclerosing Cholangitis can improve their quality of life by maintaining a healthy diet, staying active, and seeking emotional support. Ongoing research offers hope for better treatments in the future.
What is Primary Sclerosing Cholangitis?
Primary Sclerosing Cholangitis (PSC) is a rare, chronic liver disease. It affects the bile ducts, causing inflammation and scarring. This can lead to serious liver damage over time.
- PSC is an autoimmune disease, meaning the body's immune system mistakenly attacks its own cells.
- The exact cause of PSC remains unknown, though genetic and environmental factors may play a role.
- PSC primarily affects the bile ducts, which carry bile from the liver to the gallbladder and small intestine.
- Inflammation from PSC leads to scarring and narrowing of the bile ducts.
- Over time, PSC can cause liver damage, cirrhosis, and liver failure.
Symptoms of Primary Sclerosing Cholangitis
Symptoms of PSC can vary widely. Some people may have no symptoms for years, while others experience severe issues early on.
- Common symptoms include fatigue and itching.
- Jaundice, or yellowing of the skin and eyes, is another symptom.
- Abdominal pain, particularly in the upper right quadrant, can occur.
- Fever and chills may indicate an infection in the bile ducts.
- Weight loss and loss of appetite are also possible symptoms.
Diagnosis of Primary Sclerosing Cholangitis
Diagnosing PSC involves a combination of tests and procedures. Doctors look for specific signs and symptoms to confirm the disease.
- Blood tests can reveal elevated liver enzymes, indicating liver damage.
- Imaging tests, such as MRI or MRCP, help visualize the bile ducts.
- A liver biopsy may be performed to assess the extent of liver damage.
- Endoscopic retrograde cholangiopancreatography (ERCP) can provide detailed images of the bile ducts.
- Genetic testing may be used to identify potential hereditary factors.
Treatment Options for Primary Sclerosing Cholangitis
While there is no cure for PSC, various treatments can help manage symptoms and slow disease progression.
- Ursodeoxycholic acid (UDCA) is often prescribed to improve bile flow.
- Antibiotics may be used to treat or prevent infections in the bile ducts.
- Endoscopic procedures can help open narrowed bile ducts.
- Liver transplantation is an option for severe cases or liver failure.
- Immunosuppressive drugs may be used to reduce inflammation.
Complications of Primary Sclerosing Cholangitis
PSC can lead to several serious complications. Monitoring and managing these complications is crucial for patient health.
- Cirrhosis, or severe liver scarring, is a common complication.
- Liver failure can occur as the disease progresses.
- PSC increases the risk of bile duct cancer (cholangiocarcinoma).
- Gallbladder cancer risk is also higher in PSC patients.
- Portal hypertension, or increased blood pressure in the liver, can develop.
Living with Primary Sclerosing Cholangitis
Managing PSC involves regular medical care and lifestyle adjustments. Patients can take steps to improve their quality of life.
- Regular check-ups with a hepatologist are essential.
- A healthy diet can support liver function and overall health.
- Avoiding alcohol is crucial to prevent further liver damage.
- Staying active and exercising regularly can help maintain overall health.
- Support groups and counseling can provide emotional support.
Research and Future Directions
Ongoing research aims to better understand PSC and develop new treatments. Advances in science offer hope for the future.
- Clinical trials are testing new drugs to treat PSC.
- Researchers are studying the genetic factors involved in PSC.
- Advances in imaging technology are improving diagnosis and monitoring.
- Stem cell therapy is being explored as a potential treatment.
- Collaboration between researchers worldwide is accelerating progress.
Interesting Facts about Primary Sclerosing Cholangitis
PSC is a complex disease with many intriguing aspects. Here are some lesser-known facts about PSC.
- PSC is more common in men than women.
- The disease often appears between the ages of 30 and 50.
- PSC is frequently associated with inflammatory bowel disease (IBD), particularly ulcerative colitis.
- The prevalence of PSC varies by region, with higher rates in Northern Europe.
- PSC can occur in children, though it is less common.
Support and Resources for PSC Patients
Numerous organizations and resources are available to support PSC patients and their families. These can provide valuable information and assistance.
- The American Liver Foundation offers resources and support for liver disease patients.
- PSC Partners Seeking a Cure is a nonprofit organization dedicated to PSC research and support.
- Online forums and social media groups can connect patients with others facing similar challenges.
- Educational materials and webinars can help patients stay informed about their condition.
- Financial assistance programs may be available to help with medical costs.
Final Thoughts on Primary Sclerosing Cholangitis
PSC is a challenging disease, but knowledge and support can make a significant difference. Here are a few more facts to consider.
- Early diagnosis and treatment can improve outcomes for PSC patients.
- Regular monitoring is crucial to catch complications early.
- Advances in research are continually improving our understanding of PSC.
- Patient advocacy groups play a vital role in raising awareness and funding research.
- Staying informed and proactive can help PSC patients manage their condition effectively.
Final Thoughts on Primary Sclerosing Cholangitis
Primary Sclerosing Cholangitis (PSC) is a rare, chronic liver disease that affects the bile ducts. Understanding PSC is crucial for those diagnosed and their loved ones. Symptoms can vary widely, making early detection challenging. While there's no cure yet, treatments focus on managing symptoms and complications. Regular check-ups with a healthcare provider are essential for monitoring the disease's progression. Research is ongoing, offering hope for better treatments and possibly a cure in the future. Staying informed and connected with support groups can make a significant difference in managing PSC. Remember, knowledge is power when dealing with any chronic illness. Stay proactive, seek medical advice, and support research efforts. Together, we can make strides in understanding and combating PSC.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
