Primary Myelofibrosis is a rare type of bone marrow cancer that disrupts the body's ability to produce blood cells. This condition leads to extensive scarring in the bone marrow, causing severe anemia, weakness, fatigue, and often an enlarged spleen. Symptoms can vary widely, making it tricky to diagnose early. Some people might experience night sweats, fever, or bone pain. Causes of primary myelofibrosis aren't entirely understood, but genetic mutations play a significant role. Treatment options include medications, blood transfusions, and sometimes stem cell transplants. Understanding this disease is crucial for managing symptoms and improving quality of life. Let's dive into 50 facts about primary myelofibrosis to shed light on this complex condition.
Key Takeaways:
- Primary Myelofibrosis is a rare bone marrow disorder that can cause severe anemia, fatigue, and an enlarged spleen. It primarily affects individuals over 50 and is more common in men.
- Treatment for Primary Myelofibrosis focuses on managing symptoms and improving quality of life. Options include medications, blood transfusions, and stem cell transplantation, but ongoing support is crucial.
What is Primary Myelofibrosis?
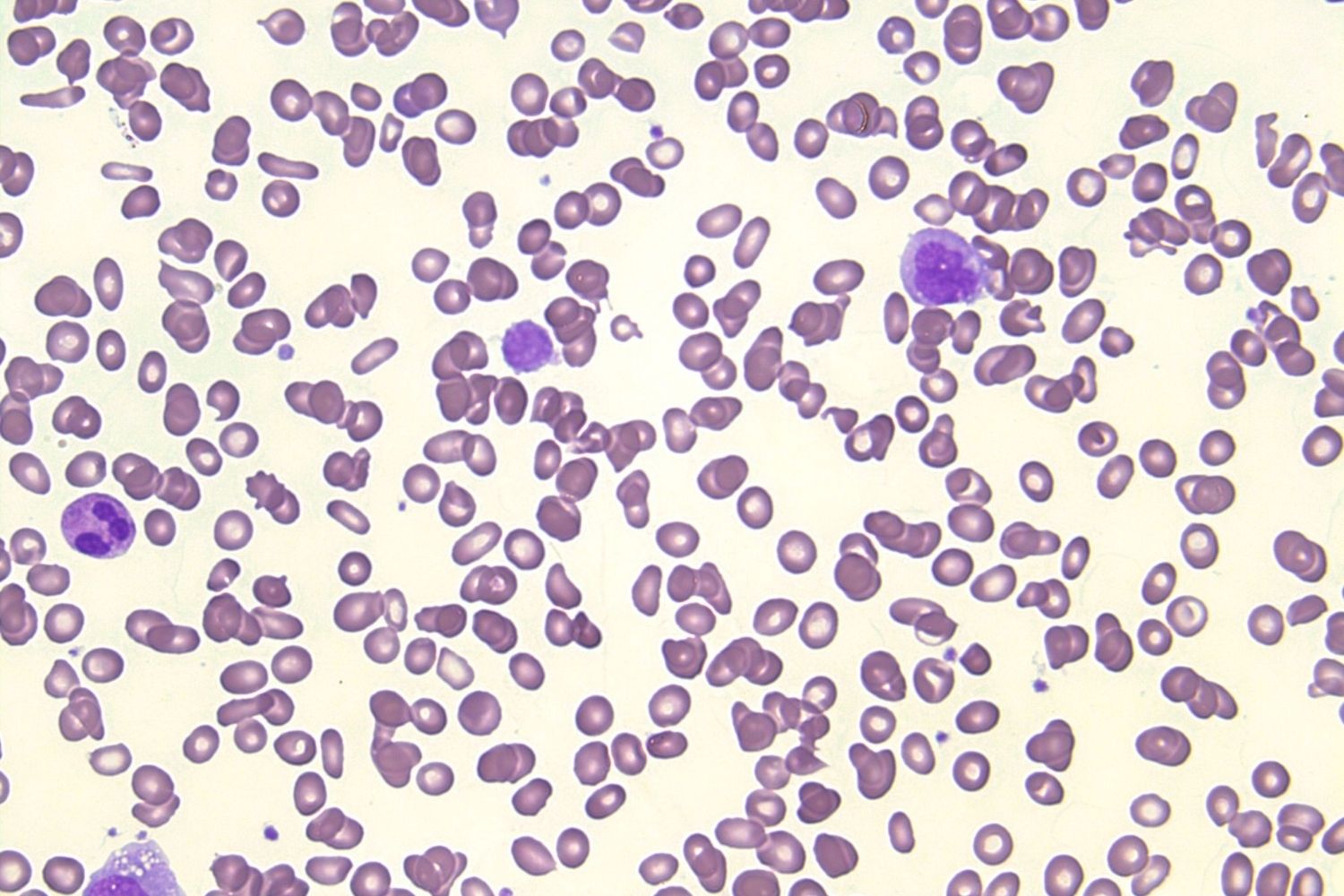
Primary Myelofibrosis (PMF) is a rare bone marrow disorder that disrupts the body's normal production of blood cells. This condition can lead to severe anemia, weakness, fatigue, and an enlarged spleen. Here are some intriguing facts about PMF.
- PMF is classified as a type of chronic leukemia.
- It is part of a group of diseases known as myeloproliferative neoplasms (MPNs).
- The exact cause of PMF remains unknown.
- PMF primarily affects individuals over the age of 50.
- Men are slightly more likely to develop PMF than women.
Symptoms of Primary Myelofibrosis
Recognizing the symptoms of PMF can be challenging as they often resemble those of other conditions. Here are some common symptoms associated with PMF.
- Fatigue is one of the most common symptoms.
- Patients often experience night sweats.
- Unexplained weight loss can occur.
- Bone pain is a frequent complaint.
- An enlarged spleen, known as splenomegaly, is a hallmark of PMF.
Diagnosis of Primary Myelofibrosis
Diagnosing PMF involves a series of tests and evaluations. Understanding these diagnostic methods can help in early detection and treatment.
- Blood tests are usually the first step in diagnosing PMF.
- A bone marrow biopsy is often required for confirmation.
- Genetic testing can identify mutations associated with PMF.
- Imaging tests like ultrasound or MRI may be used to assess spleen size.
- A complete blood count (CBC) is essential for monitoring blood cell levels.
Causes and Risk Factors
While the exact cause of PMF is unknown, several risk factors and genetic mutations have been identified.
- Mutations in the JAK2 gene are found in about 50% of PMF cases.
- CALR and MPL gene mutations are also linked to PMF.
- Exposure to certain chemicals or radiation may increase the risk.
- Family history of MPNs can be a risk factor.
- Chronic inflammation is thought to play a role in PMF development.
Treatment Options for Primary Myelofibrosis
Treatment for PMF focuses on managing symptoms and improving quality of life. Here are some common treatment options.
- Medications like ruxolitinib can help reduce spleen size and alleviate symptoms.
- Blood transfusions may be necessary to manage anemia.
- Hydroxyurea is often used to control blood cell production.
- Stem cell transplantation offers a potential cure but carries significant risks.
- Supportive care, including pain management and nutritional support, is crucial.
Complications of Primary Myelofibrosis
PMF can lead to various complications that impact overall health. Understanding these complications is vital for managing the disease.
- Severe anemia can result from PMF.
- Patients are at increased risk of infections.
- PMF can progress to acute myeloid leukemia (AML).
- Portal hypertension may develop due to an enlarged spleen.
- Bone marrow fibrosis can lead to bone marrow failure.
Living with Primary Myelofibrosis
Living with PMF requires ongoing management and support. Here are some tips for coping with the condition.
- Regular follow-up appointments are essential.
- Maintaining a healthy diet can help manage symptoms.
- Exercise, within limits, can improve overall well-being.
- Support groups provide emotional and practical support.
- Staying informed about the latest research and treatments is beneficial.
Research and Future Directions
Ongoing research aims to improve the understanding and treatment of PMF. Here are some exciting developments in the field.
- New medications targeting specific genetic mutations are being developed.
- Clinical trials are exploring innovative treatment approaches.
- Researchers are investigating the role of the immune system in PMF.
- Advances in genetic testing are improving diagnostic accuracy.
- Personalized medicine is becoming a reality for PMF patients.
Statistics and Epidemiology
Understanding the prevalence and impact of PMF can provide valuable insights into the disease.
- PMF affects approximately 1 in 100,000 people.
- The median survival rate for PMF patients is around 5-7 years.
- Early diagnosis and treatment can improve prognosis.
- PMF is more common in developed countries.
- The incidence of PMF is increasing, possibly due to better diagnostic techniques.
Support and Resources
Various organizations and resources are available to support PMF patients and their families.
- The Leukemia & Lymphoma Society offers resources and support.
- The MPN Research Foundation funds research and provides patient support.
- Online forums and support groups connect patients and caregivers.
- Educational materials and webinars are available for patients.
- Advocacy groups work to raise awareness and improve patient care.
Final Thoughts on Primary Myelofibrosis
Primary Myelofibrosis (PMF) is a rare but serious bone marrow disorder. It disrupts normal blood cell production, leading to symptoms like fatigue, anemia, and an enlarged spleen. Understanding PMF helps in early diagnosis and better management. Treatments range from medications to stem cell transplants, offering hope to patients. Staying informed about the latest research and treatment options is crucial for those affected. Support from healthcare providers, family, and patient communities can make a significant difference. Remember, while PMF poses challenges, advancements in medical science continue to improve outcomes. Always consult with a healthcare professional for personalized advice and treatment plans. Knowledge empowers patients and caregivers alike, fostering a proactive approach to managing this condition.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
