Posterior Urethral Valves (PUV) are a rare but serious condition affecting the urinary tract in male infants. These abnormal folds of tissue in the urethra can block urine flow, leading to kidney damage and other complications. Early diagnosis and treatment are crucial for managing this condition effectively. Symptoms might include difficulty urinating, a weak urine stream, or urinary tract infections. Ultrasounds and voiding cystourethrograms (VCUG) are common diagnostic tools. Treatment often involves surgical intervention to remove or bypass the obstructive tissue. Understanding PUV can help parents and caregivers recognize symptoms early, ensuring timely medical attention. This article will provide 50 essential facts about PUV, offering a comprehensive overview of its causes, symptoms, diagnosis, and treatment options.
Key Takeaways:
- Posterior Urethral Valves (PUV) is a rare condition in male infants, causing urinary tract issues. Early detection and treatment are crucial to prevent kidney damage and other complications.
- Managing PUV involves surgical and medical interventions, regular monitoring, and lifestyle adjustments. With proper care, many children can lead healthy lives, but ongoing challenges may require support and advocacy.
Understanding Posterior Urethral Valves
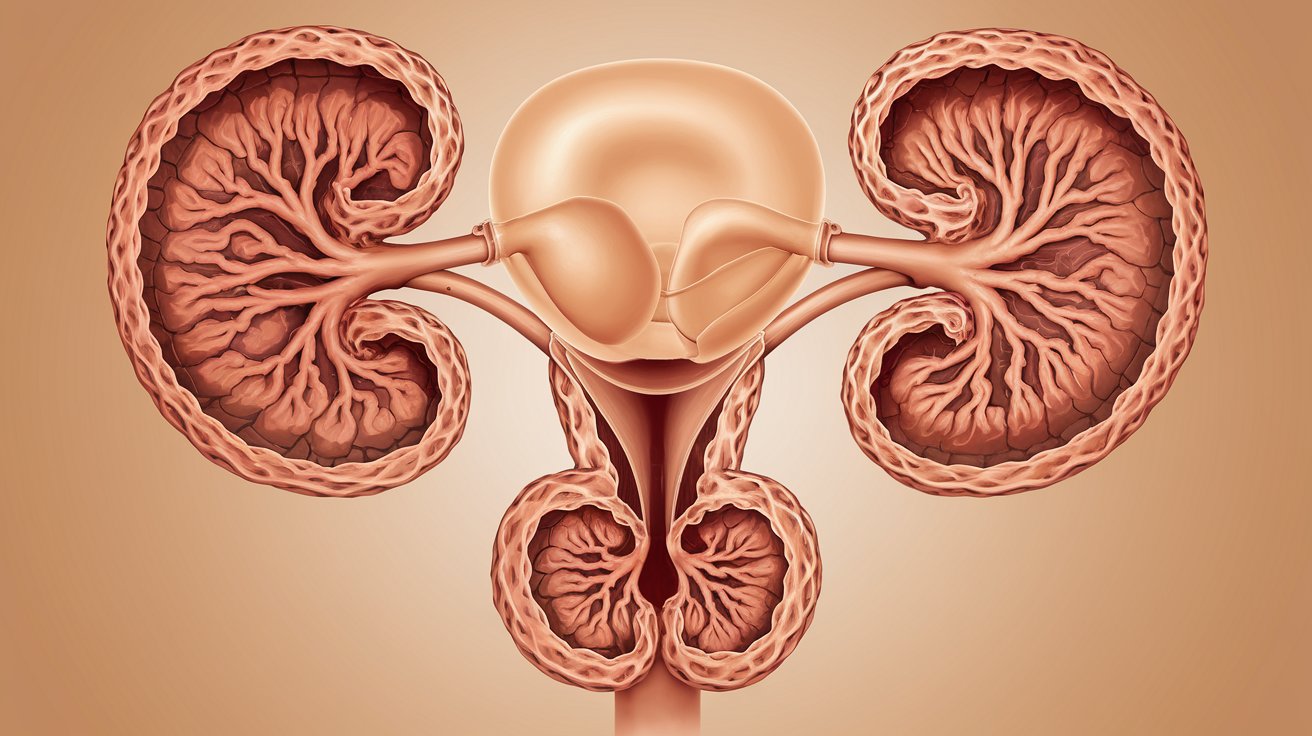
Posterior Urethral Valves (PUV) is a rare condition affecting the urinary tract of male infants. It involves the presence of abnormal flaps of tissue in the urethra, which can obstruct urine flow. Here are some intriguing facts about this condition:
-
PUV is a congenital condition: This means it is present at birth and develops during fetal growth.
-
Only affects males: PUV exclusively occurs in male infants due to the anatomical structure of the male urethra.
-
Incidence rate: It affects approximately 1 in 8,000 male births.
-
Detected via ultrasound: Often, PUV is identified during a routine prenatal ultrasound.
-
Causes bladder distension: The obstruction can lead to an enlarged bladder, which can be seen on ultrasound.
-
Can cause kidney damage: If untreated, PUV can lead to significant kidney damage due to back pressure.
-
Symptoms in newborns: These may include difficulty urinating, a weak urine stream, and urinary tract infections.
-
Vesicoureteral reflux: This condition often accompanies PUV, where urine flows backward from the bladder to the kidneys.
-
Hydronephrosis: Swelling of the kidneys due to urine buildup is another common complication.
-
Diagnosis post-birth: A voiding cystourethrogram (VCUG) is often used to diagnose PUV after birth.
Treatment Options for PUV
Managing PUV involves a combination of medical and surgical interventions. Early detection and treatment are crucial for preventing long-term complications.
-
Endoscopic valve ablation: This is the most common surgical treatment, where the obstructing tissue is removed using a cystoscope.
-
Vesicostomy: In severe cases, a temporary opening is made in the bladder to allow urine to bypass the obstruction.
-
Antibiotic prophylaxis: To prevent urinary tract infections, antibiotics may be prescribed.
-
Regular monitoring: Post-surgery, children require regular follow-ups to monitor kidney function and bladder health.
-
Hydration: Ensuring adequate fluid intake helps maintain urinary flow and prevent infections.
-
Bladder training: Techniques to improve bladder control and function may be recommended as the child grows.
-
Kidney function tests: Regular blood tests are necessary to assess kidney health.
-
Ultrasound scans: Periodic ultrasounds help monitor the condition of the kidneys and bladder.
-
Urodynamic studies: These tests evaluate how well the bladder and urethra are storing and releasing urine.
-
Parental education: Parents are taught signs of urinary issues and the importance of follow-up care.
Long-term Outlook for Children with PUV
With proper treatment and monitoring, many children with PUV can lead healthy lives. However, some may face ongoing challenges.
-
Chronic kidney disease: Some children may develop chronic kidney disease due to prolonged back pressure on the kidneys.
-
Bladder dysfunction: Issues like overactive bladder or incontinence can persist.
-
Growth and development: Regular check-ups ensure that growth and development are on track.
-
Psychosocial support: Counseling may be beneficial for children and families coping with chronic health issues.
-
School accommodations: Some children may need special accommodations at school for bathroom breaks.
-
Transition to adult care: As they age, transitioning to adult urology care is important for continued health management.
-
Genetic counseling: Families may benefit from genetic counseling to understand the risk of PUV in future pregnancies.
-
Research and advancements: Ongoing research aims to improve diagnosis, treatment, and outcomes for PUV.
-
Support groups: Connecting with other families facing similar challenges can provide emotional support and practical advice.
-
Awareness and advocacy: Raising awareness about PUV can help improve early detection and treatment.
Complications Associated with PUV
Despite treatment, PUV can lead to several complications that require ongoing management.
-
Urinary incontinence: Some children may struggle with controlling urine flow.
-
Recurrent UTIs: Frequent urinary tract infections can occur, necessitating vigilant monitoring.
-
Bladder stones: The risk of bladder stones increases due to urinary stasis.
-
Electrolyte imbalances: Kidney dysfunction can lead to imbalances in electrolytes like sodium and potassium.
-
High blood pressure: Kidney damage can result in hypertension, requiring medication and lifestyle changes.
-
Proteinuria: The presence of protein in urine indicates kidney damage and needs regular monitoring.
-
Growth retardation: Chronic kidney disease can impact a child's growth and development.
-
Anemia: Kidney issues can lead to anemia, requiring treatment with iron supplements or erythropoietin.
-
Bone health: Kidney disease can affect bone health, necessitating calcium and vitamin D supplements.
-
Dialysis or transplant: In severe cases, children may require dialysis or a kidney transplant.
Preventive Measures and Lifestyle Adjustments
While PUV cannot be prevented, certain measures can help manage the condition and improve quality of life.
-
Healthy diet: A balanced diet supports overall health and kidney function.
-
Regular exercise: Physical activity promotes general well-being and can help manage blood pressure.
-
Avoiding nephrotoxic drugs: Certain medications can harm the kidneys and should be avoided.
-
Hydration: Drinking plenty of fluids helps maintain urinary tract health.
-
Routine check-ups: Regular medical visits ensure early detection of any complications.
-
Parental vigilance: Parents should watch for signs of urinary issues and seek prompt medical attention.
-
Education and awareness: Understanding the condition helps families manage it more effectively.
-
Support networks: Engaging with support groups and healthcare professionals provides valuable resources.
-
Mental health care: Addressing emotional and psychological needs is crucial for the child's overall well-being.
-
Advocacy: Advocating for better healthcare resources and research funding can improve outcomes for children with PUV.
Final Thoughts on Posterior Urethral Valves
Posterior urethral valves (PUV) are a serious condition affecting young boys, causing urinary tract obstruction. Early diagnosis and treatment are crucial for preventing long-term kidney damage. Symptoms like difficulty urinating, urinary tract infections, and poor growth should prompt immediate medical attention. Treatment often involves surgical intervention to remove the obstructive valves, improving urinary flow and kidney function.
Parents and caregivers must stay informed about PUV and work closely with healthcare providers to manage the condition effectively. Regular follow-ups and monitoring are essential to ensure the child's health and well-being. Understanding the importance of early detection and intervention can make a significant difference in the quality of life for children with PUV. By staying vigilant and proactive, families can navigate the challenges of PUV and support their child's health journey.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
