Polyarteritis Nodosa is a rare but serious disease that affects small and medium-sized arteries, causing them to become inflamed and damaged. This condition can lead to a variety of symptoms, depending on which organs are affected. Common symptoms include fever, weight loss, muscle pain, and fatigue. The exact cause of Polyarteritis Nodosa remains unknown, but it is believed to be related to the immune system attacking the blood vessels. Early diagnosis and treatment are crucial to managing the disease and preventing severe complications. Treatments often involve medications to reduce inflammation and suppress the immune system. Understanding the key facts about Polyarteritis Nodosa can help patients and their families navigate this challenging condition.
Key Takeaways:
- Polyarteritis Nodosa is a rare autoimmune disease that can affect any organ system and requires prompt treatment to improve prognosis.
- Patients with Polyarteritis Nodosa can benefit from a combination of medications, lifestyle adjustments, and support from healthcare providers and loved ones.
What is Polyarteritis Nodosa?
Polyarteritis Nodosa (PAN) is a rare autoimmune disease that causes inflammation of small and medium-sized arteries. This inflammation can lead to organ damage and various symptoms. Here are some intriguing facts about PAN.
- PAN primarily affects middle-aged adults but can occur at any age.
- The exact cause of PAN remains unknown, though it’s believed to involve an abnormal immune response.
- PAN can affect any organ system, including the skin, kidneys, heart, and nervous system.
- Symptoms vary widely but often include fever, weight loss, and muscle pain.
- PAN is more common in men than women.
- The disease can be life-threatening if not treated promptly.
- PAN is often diagnosed through a combination of blood tests, imaging studies, and biopsies.
- Treatment typically involves corticosteroids and immunosuppressive drugs.
- PAN can cause aneurysms, which are abnormal bulges in blood vessels.
- The disease may be associated with hepatitis B or C infections.
Symptoms and Diagnosis
Understanding the symptoms and how PAN is diagnosed can help in early detection and treatment.
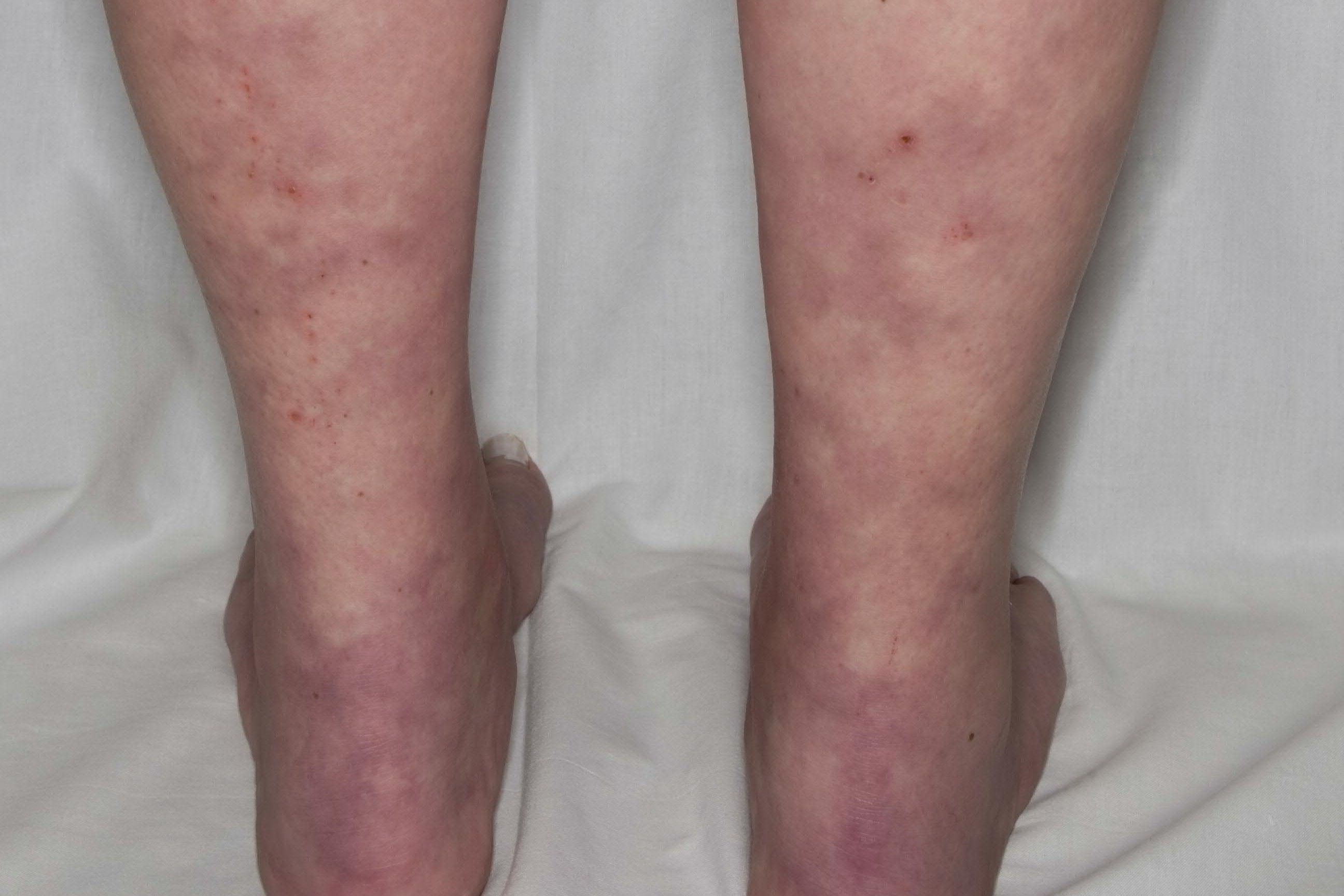
- Common skin symptoms include rashes, ulcers, and nodules.
- PAN can cause severe abdominal pain due to inflammation of the arteries supplying the intestines.
- Kidney involvement can lead to high blood pressure and kidney failure.
- Nerve damage from PAN can result in numbness, tingling, or weakness.
- Some patients experience heart problems, such as heart attacks or heart failure.
- Blood tests may show elevated inflammatory markers like ESR and CRP.
- Angiography, an imaging test, can reveal characteristic changes in blood vessels.
- A biopsy of affected tissue can confirm the diagnosis by showing inflamed arteries.
- Early diagnosis and treatment improve the prognosis for PAN patients.
- Misdiagnosis is common due to the disease’s varied symptoms.
Treatment and Management
Effective management of PAN involves a combination of medications and lifestyle adjustments.
- Corticosteroids like prednisone are often the first line of treatment.
- Immunosuppressive drugs such as cyclophosphamide may be used for severe cases.
- Regular monitoring is essential to adjust treatment and manage side effects.
- Patients should avoid infections, as immunosuppressive therapy can weaken the immune system.
- Blood pressure control is crucial to prevent complications.
- Pain management strategies may include medications and physical therapy.
- Some patients benefit from plasmapheresis, a procedure that removes antibodies from the blood.
- Lifestyle changes, such as a healthy diet and regular exercise, can support overall health.
- Psychological support is important, as chronic illness can affect mental health.
- Patients should work closely with a multidisciplinary team of healthcare providers.
Prognosis and Research
Research continues to improve our understanding of PAN and develop better treatments.
- The prognosis for PAN has improved significantly with modern treatments.
- Some patients achieve long-term remission, while others may have relapses.
- Ongoing research aims to identify genetic factors that may contribute to PAN.
- Clinical trials are testing new medications and treatment approaches.
- Patient registries help researchers collect data on the disease’s progression and outcomes.
- Advances in imaging technology improve the ability to diagnose and monitor PAN.
- Collaboration between researchers and patient advocacy groups raises awareness and funding.
- Understanding the role of the immune system in PAN may lead to targeted therapies.
- Research into related diseases, like other forms of vasculitis, can provide insights into PAN.
- Patients can participate in research studies to contribute to scientific knowledge.
Living with Polyarteritis Nodosa
Living with PAN requires ongoing management and support from healthcare providers, family, and friends.
- Patients should educate themselves about the disease to make informed decisions.
- Support groups can provide emotional and practical support.
- Regular follow-up appointments are necessary to monitor the disease and adjust treatment.
- Patients should report new or worsening symptoms to their healthcare provider promptly.
- Maintaining a healthy lifestyle can improve overall well-being and disease outcomes.
- Patients may need to make adjustments to their work or daily activities.
- Stress management techniques, such as meditation or counseling, can be beneficial.
- Family members should be educated about PAN to provide effective support.
- Patients should keep a medical journal to track symptoms, medications, and appointments.
- Open communication with healthcare providers is key to managing the disease effectively.
Final Thoughts on Polyarteritis Nodosa
Polyarteritis Nodosa (PAN) is a rare but serious disease that affects small and medium-sized arteries, causing inflammation and damage. Understanding the symptoms, which can range from fever and fatigue to muscle pain and skin rashes, is crucial for early diagnosis. Treatment often involves corticosteroids and immunosuppressive drugs to manage inflammation and prevent further complications. While PAN can be life-threatening, early detection and proper medical care can significantly improve outcomes. Awareness and education about this condition are essential for both patients and healthcare providers. Remember, if you or someone you know is experiencing unexplained symptoms, consult a healthcare professional for a thorough evaluation. Knowledge is power, and staying informed can make all the difference in managing this complex disease.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
