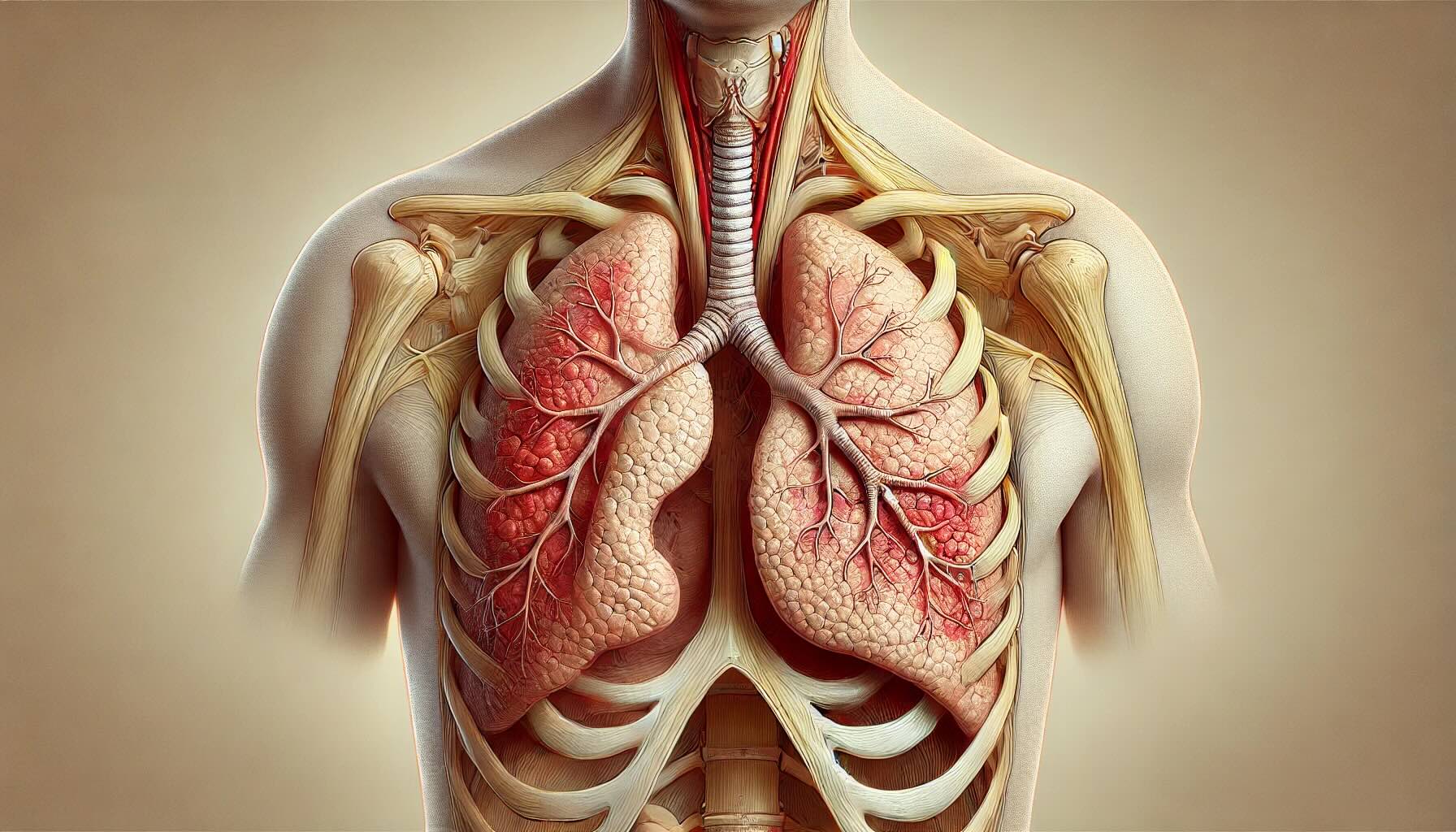
Pleuritis, also known as pleurisy, is a condition where the pleura, the thin layers of tissue surrounding the lungs, become inflamed. This inflammation can cause sharp chest pain that worsens during breathing. Pleuritis often results from infections, such as pneumonia or tuberculosis, but can also be linked to autoimmune diseases, lung cancer, or chest injuries. Symptoms include chest pain, shortness of breath, and a dry cough. Diagnosing pleuritis typically involves imaging tests like X-rays or CT scans, along with blood tests to identify underlying causes. Treatment focuses on addressing the root cause and relieving pain, often using anti-inflammatory medications. Understanding pleuritis is crucial for managing its symptoms and preventing complications.
Key Takeaways:
- Pleuritis, or pleurisy, is chest pain caused by lung membrane inflammation. It can be triggered by infections, autoimmune diseases, or chest trauma. Treatment includes rest, pain relievers, and breathing exercises.
- Early diagnosis and treatment of pleuritis improve the prognosis significantly. Lifestyle changes, vaccinations, and maintaining a healthy immune system can help prevent this condition.
What is Pleuritis?
Pleuritis, also known as pleurisy, is an inflammation of the pleura, the double-layered membrane surrounding the lungs. This condition can cause sharp chest pain that worsens during breathing. Here are some intriguing facts about pleuritis.
- Pleuritis can be caused by viral infections, bacterial infections, or even fungi.
- Autoimmune diseases like lupus and rheumatoid arthritis can also lead to pleuritis.
- Chest trauma or injury can trigger pleuritis.
- Certain medications, such as those used in chemotherapy, may cause pleuritis as a side effect.
- Pleuritis can sometimes be a complication of pneumonia.
- Tuberculosis is a less common but serious cause of pleuritis.
- Pleuritis can occur in people of all ages, but it is more common in adults.
- The pain from pleuritis is often described as stabbing or sharp.
- Pain typically worsens with deep breaths, coughing, or sneezing.
- Shortness of breath is a common symptom of pleuritis.
- Fever and chills may accompany pleuritis if an infection is present.
- A dry cough is another symptom often associated with pleuritis.
- Pleural effusion, the buildup of fluid between the pleura, can occur with pleuritis.
- Imaging tests like X-rays and CT scans help diagnose pleuritis.
- Blood tests can identify underlying infections or autoimmune conditions causing pleuritis.
- Ultrasound may be used to detect pleural effusion.
- Thoracentesis, a procedure to remove fluid from the pleural space, can help diagnose and treat pleuritis.
- Anti-inflammatory medications are commonly used to treat pleuritis.
- Antibiotics are prescribed if a bacterial infection is the cause.
- In severe cases, corticosteroids may be used to reduce inflammation.
Symptoms and Diagnosis
Understanding the symptoms and how pleuritis is diagnosed can help in managing the condition effectively.
- The hallmark symptom of pleuritis is sharp chest pain.
- Pain may radiate to the shoulder or back.
- Breathing deeply, coughing, or sneezing can exacerbate the pain.
- Some people experience a dull, aching pain instead of sharp pain.
- Listening to the lungs with a stethoscope can reveal a pleural friction rub, a sign of pleuritis.
- Blood tests can show elevated white blood cell counts, indicating infection or inflammation.
- Elevated levels of C-reactive protein (CRP) in the blood can also indicate inflammation.
- Arterial blood gas tests can measure oxygen and carbon dioxide levels in the blood.
- Spirometry tests can assess lung function and capacity.
- A biopsy of the pleura may be performed if cancer is suspected.
Treatment and Management
Effective treatment and management strategies can significantly improve the quality of life for those with pleuritis.
- Rest is crucial for recovery from pleuritis.
- Over-the-counter pain relievers like ibuprofen can help manage pain.
- Applying heat or cold packs to the chest can provide relief.
- Breathing exercises can help maintain lung function.
- In cases of pleural effusion, draining the fluid can alleviate symptoms.
- Oxygen therapy may be needed if breathing is severely affected.
- Lifestyle changes, such as quitting smoking, can help prevent pleuritis.
- Staying hydrated is important for overall lung health.
- Avoiding exposure to respiratory irritants can reduce the risk of pleuritis.
- Regular follow-up appointments with a healthcare provider are essential for monitoring the condition.
Complications and Prognosis
While pleuritis can be painful and uncomfortable, understanding potential complications and the prognosis can help in managing expectations.
- Untreated pleuritis can lead to chronic pain and discomfort.
- Pleural effusion can cause significant breathing difficulties.
- In rare cases, pleuritis can lead to pleural thickening, which restricts lung expansion.
- Empyema, a collection of pus in the pleural space, is a serious complication.
- Sepsis, a life-threatening infection, can occur if pleuritis is caused by a severe bacterial infection.
- Most cases of pleuritis resolve with proper treatment.
- Early diagnosis and treatment improve the prognosis significantly.
- Chronic pleuritis may require long-term management strategies.
- Vaccinations, such as the flu and pneumonia vaccines, can help prevent infections that cause pleuritis.
- Maintaining a healthy immune system through diet and exercise can reduce the risk of pleuritis.
Final Thoughts on Pleuritis
Pleuritis, or pleurisy, is an inflammation of the pleura, the membrane surrounding the lungs. This condition can cause sharp chest pain, especially when breathing deeply or coughing. Common causes include infections, autoimmune diseases, and injuries. Symptoms often mimic other conditions, making diagnosis tricky. Treatment usually involves addressing the underlying cause, pain management, and sometimes antibiotics or anti-inflammatory medications.
Understanding pleuritis is crucial for early detection and effective treatment. If you experience persistent chest pain, seek medical advice promptly. Early intervention can prevent complications and improve outcomes. Stay informed, listen to your body, and don't hesitate to consult healthcare professionals when in doubt. Knowledge is power, and being aware of conditions like pleuritis can make a significant difference in your health journey.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
