Phosphomannoisomerase Deficiency, also known as MPI-CDG, is a rare genetic disorder that affects the body's ability to process certain sugars. This condition can lead to a variety of symptoms, including developmental delays, liver problems, and gastrointestinal issues. Caused by mutations in the MPI gene, this deficiency disrupts the normal function of the enzyme phosphomannose isomerase, which is crucial for glycosylation—a process essential for the proper functioning of many proteins. Early diagnosis and treatment are vital for managing symptoms and improving quality of life. In this blog post, we'll explore 50 intriguing facts about this rare condition, shedding light on its causes, symptoms, and potential treatments.
Key Takeaways:
- Phosphomannoisomerase Deficiency, or MPI-CDG, is a rare genetic disorder affecting sugar processing. It can cause various symptoms from infancy, but early diagnosis and management are crucial for improving quality of life.
- Diagnosis involves genetic testing, enzyme activity assays, and clinical evaluations. While there's no cure, treatments like dietary management and supportive therapies can help manage symptoms and improve overall well-being.
What is Phosphomannoisomerase Deficiency?
Phosphomannoisomerase Deficiency, also known as MPI-CDG, is a rare genetic disorder. It affects the body's ability to process certain sugars, leading to a variety of health issues. Let's dive into some fascinating facts about this condition.
-
Genetic Origin: This disorder is inherited in an autosomal recessive manner, meaning both parents must carry the defective gene.
-
Enzyme Deficiency: The condition results from a deficiency in the enzyme phosphomannose isomerase (PMI), crucial for glycoprotein synthesis.
-
Glycosylation Disorder: MPI-CDG is classified as a congenital disorder of glycosylation (CDG), impacting the glycosylation process in cells.
-
Rare Occurrence: It's extremely rare, with only a few dozen cases reported worldwide.
-
Symptoms Vary: Symptoms can range from mild to severe, including developmental delays, liver dysfunction, and gastrointestinal issues.
-
Early Onset: Symptoms often appear in infancy or early childhood, making early diagnosis critical.
-
Growth Issues: Many affected children experience growth retardation and failure to thrive.
-
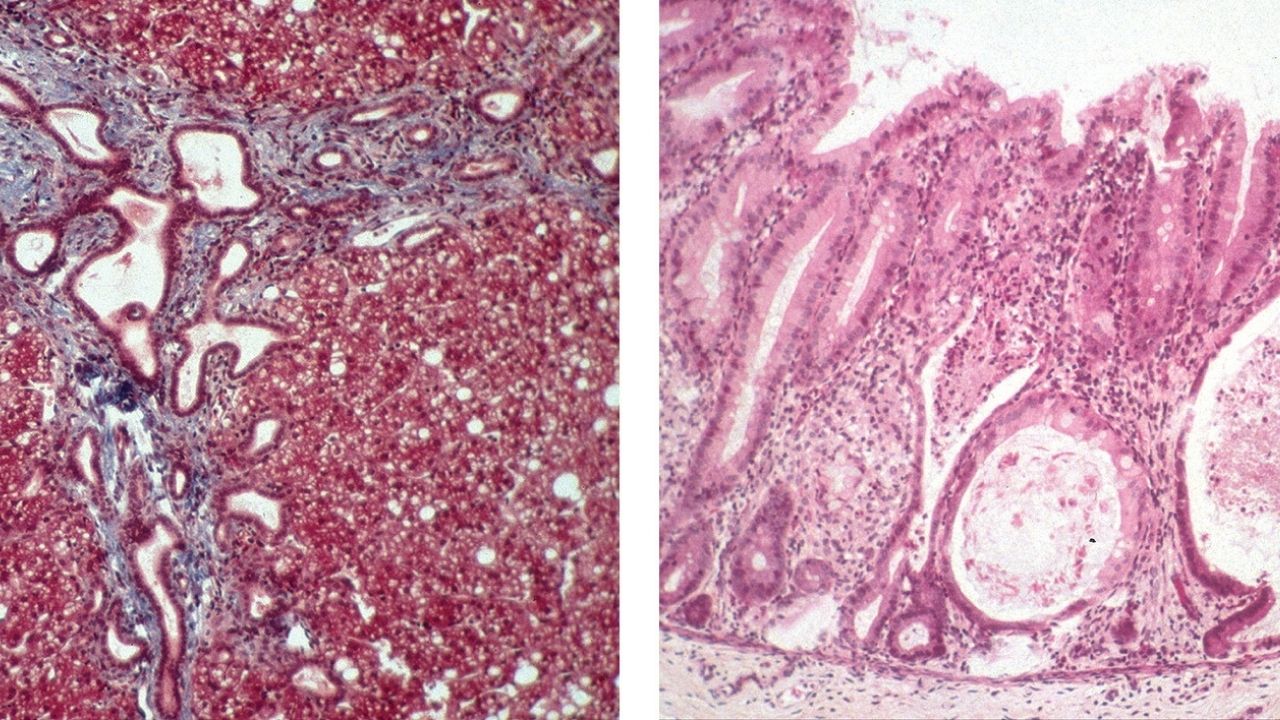
Liver Complications: Liver problems, such as hepatomegaly (enlarged liver) and liver fibrosis, are common.
-
Gastrointestinal Problems: Chronic diarrhea and protein-losing enteropathy are frequent gastrointestinal issues.
-
Neurological Impact: Some patients may have neurological symptoms like hypotonia (low muscle tone) and developmental delays.
Diagnosis and Testing
Diagnosing MPI-CDG involves several tests and evaluations. Understanding these can help in early detection and management.
-
Genetic Testing: Confirmatory diagnosis is typically made through genetic testing to identify mutations in the MPI gene.
-
Enzyme Activity Assay: Measuring PMI enzyme activity in blood or fibroblasts can support the diagnosis.
-
Biochemical Tests: Blood tests may reveal abnormal glycosylation patterns, indicating a CDG.
-
Liver Biopsy: In some cases, a liver biopsy may be performed to assess liver damage and fibrosis.
-
Prenatal Testing: For families with a known history, prenatal genetic testing is available.
-
Newborn Screening: Some regions include CDG screening in their newborn screening programs.
-
Clinical Evaluation: A thorough clinical evaluation, including growth and developmental assessments, is essential.
-
Family History: A detailed family history can provide clues and support the diagnosis.
-
Metabolic Tests: Additional metabolic tests may be conducted to rule out other conditions.
-
Multidisciplinary Approach: Diagnosis often involves a team of specialists, including geneticists, hepatologists, and neurologists.
Treatment and Management
While there's no cure for MPI-CDG, various treatments can help manage symptoms and improve quality of life.
-
Dietary Management: A high-protein, low-carbohydrate diet can help manage gastrointestinal symptoms.
-
Mannose Supplementation: Oral mannose supplements can improve glycosylation and alleviate some symptoms.
-
Liver Transplant: In severe cases of liver disease, a liver transplant may be considered.
-
Supportive Therapies: Physical, occupational, and speech therapies can aid in developmental progress.
-
Regular Monitoring: Ongoing monitoring of liver function and growth is crucial.
-
Nutritional Support: Nutritional support, including supplements and specialized diets, can help maintain health.
-
Symptomatic Treatment: Treating specific symptoms, such as diarrhea or liver issues, is essential.
-
Genetic Counseling: Families may benefit from genetic counseling to understand the condition and its inheritance.
-
Patient Education: Educating patients and families about the condition and its management is vital.
-
Research Participation: Participation in clinical trials and research studies can provide access to new treatments.
Living with MPI-CDG
Living with MPI-CDG presents unique challenges. Awareness and support can make a significant difference.
-
Support Groups: Joining support groups can provide emotional support and practical advice.
-
Educational Plans: Individualized education plans (IEPs) can help children succeed in school.
-
Medical Alert: Wearing a medical alert bracelet can be lifesaving in emergencies.
-
Regular Check-ups: Regular medical check-ups are essential to monitor health and adjust treatments.
-
Mental Health: Addressing mental health needs, including counseling, is important for overall well-being.
-
Community Resources: Utilizing community resources and services can provide additional support.
-
Advocacy: Advocacy for rare diseases can help raise awareness and improve resources.
-
Financial Planning: Financial planning can help manage the costs associated with ongoing medical care.
-
Care Coordination: Coordinating care among various specialists ensures comprehensive management.
-
Quality of Life: Focusing on quality of life and enjoying activities can improve overall happiness.
Research and Future Directions
Research continues to advance our understanding of MPI-CDG. Staying informed about new developments is key.
-
Gene Therapy: Research into gene therapy holds promise for future treatments.
-
Clinical Trials: Ongoing clinical trials are exploring new therapies and interventions.
-
Biomarker Discovery: Identifying new biomarkers can improve diagnosis and monitoring.
-
Patient Registries: Patient registries help collect data and support research efforts.
-
International Collaboration: International collaboration among researchers accelerates progress.
-
Funding and Grants: Increased funding and grants support research initiatives.
-
Public Awareness: Raising public awareness can drive research and support.
-
Advancements in Genetics: Advances in genetic research may lead to new insights and treatments.
-
Personalized Medicine: Personalized medicine approaches can tailor treatments to individual needs.
-
Hope for the Future: Continued research offers hope for better treatments and outcomes for those with MPI-CDG.
Final Note on Phosphomannoisomerase Deficiency
Phosphomannoisomerase Deficiency, also known as MPI-CDG, is a rare genetic disorder that affects the body's ability to process certain sugars. This condition can lead to a variety of symptoms, including developmental delays, liver problems, and gastrointestinal issues. Early diagnosis and treatment are crucial for managing the symptoms and improving the quality of life for those affected.
Understanding the genetic basis and the biochemical pathways involved in MPI-CDG can help in developing targeted therapies. Researchers are continually exploring new treatments and interventions to better support patients and their families.
If you or someone you know is affected by this condition, it's important to seek medical advice and support from healthcare professionals who specialize in genetic disorders. Staying informed and connected with support groups can also provide valuable resources and emotional support.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
