Periventricular Leukomalacia (PVL) is a brain injury that primarily affects premature infants. This condition involves the death of small areas of brain tissue around fluid-filled spaces called ventricles. PVL can lead to motor control issues, developmental delays, and other neurological problems. Understanding PVL is crucial for parents, caregivers, and medical professionals who work with premature babies. This blog post will provide 50 essential facts about Periventricular Leukomalacia, covering its causes, symptoms, diagnosis, treatment options, and long-term effects. Whether you're a concerned parent or a curious student, these facts will offer valuable insights into this complex condition.
Key Takeaways:
- Periventricular Leukomalacia (PVL) is a brain injury that affects premature babies, leading to developmental issues. Early diagnosis and supportive therapies can improve the quality of life for affected children.
- Research and advocacy efforts are ongoing to better understand PVL, develop new treatments, and raise awareness. Families can find support through organizations and personal stories, offering hope and valuable insights.
What is Periventricular Leukomalacia?
Periventricular Leukomalacia (PVL) is a type of brain injury that affects premature infants. It involves the death of small areas of brain tissue around the ventricles, which are fluid-filled spaces in the brain. This condition can lead to various developmental issues.
- PVL primarily affects premature babies born before 32 weeks of gestation.
- The condition is characterized by the softening of white brain tissue near the ventricles.
- PVL can result from a lack of oxygen or blood flow to the brain.
- It is one of the leading causes of cerebral palsy in premature infants.
- The condition is more common in twins and multiple births.
Causes and Risk Factors
Understanding the causes and risk factors of PVL can help in early diagnosis and management. Several factors contribute to the development of this condition.
- Infections during pregnancy can increase the risk of PVL.
- Maternal health issues like preeclampsia are linked to higher PVL rates.
- Intrauterine growth restriction (IUGR) is another risk factor.
- Chorioamnionitis, an infection of the fetal membranes, can lead to PVL.
- Premature rupture of membranes (PROM) is also associated with PVL.
Symptoms and Diagnosis
Recognizing the symptoms early can lead to better management of PVL. Diagnosis often involves various imaging techniques and clinical evaluations.
- Symptoms may include developmental delays and motor skill issues.
- Seizures can be a sign of PVL in infants.
- Muscle stiffness or spasticity is another common symptom.
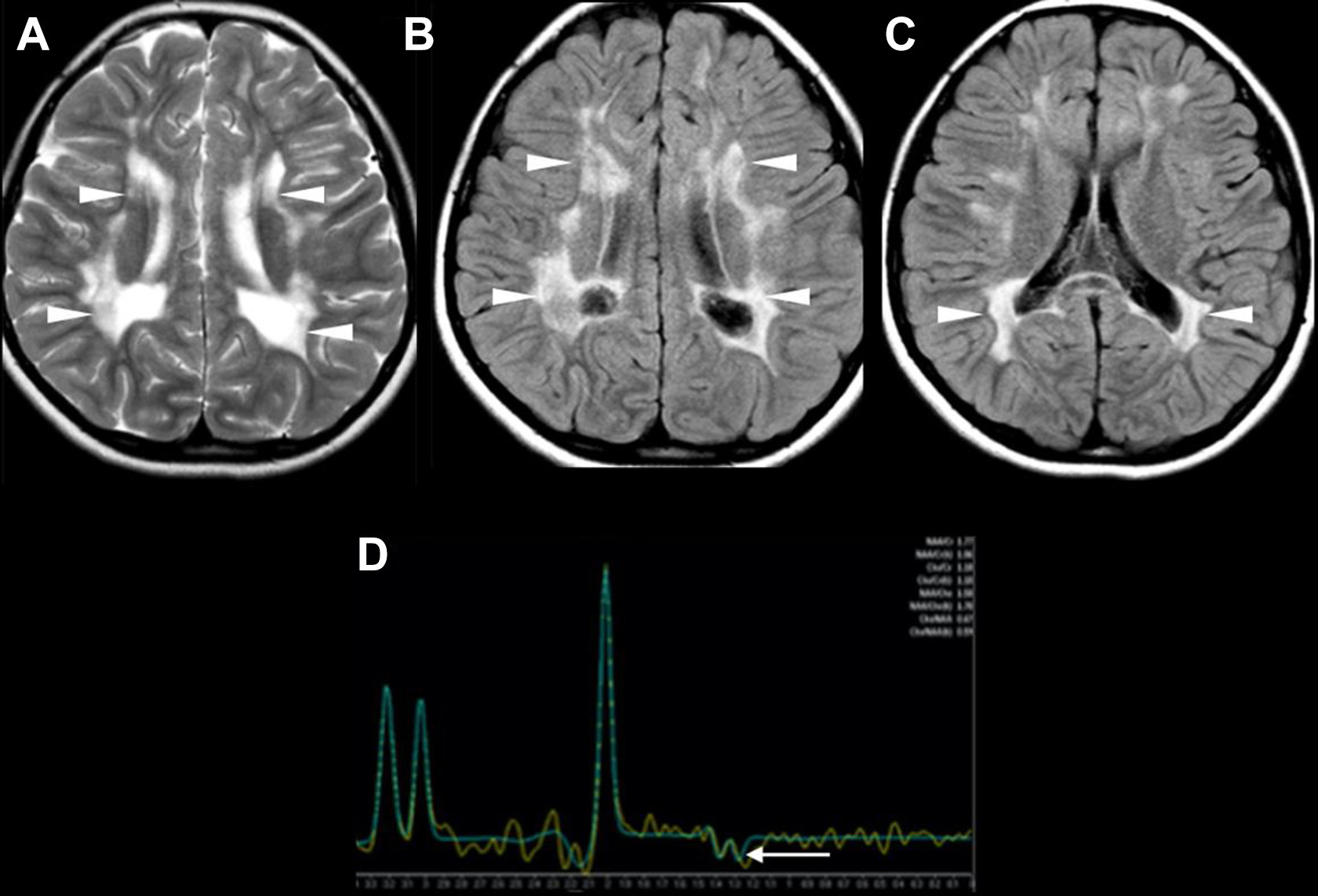
- MRI scans are often used to diagnose PVL.
- Cranial ultrasounds can also help in identifying PVL.
Treatment and Management
While there is no cure for PVL, various treatments can help manage the symptoms and improve quality of life. Early intervention is crucial.
- Physical therapy can aid in improving motor skills.
- Occupational therapy helps with daily activities and fine motor skills.
- Speech therapy can assist with communication difficulties.
- Medications may be prescribed to manage seizures.
- Regular follow-ups with a pediatric neurologist are essential.
Long-term Effects
PVL can have long-term effects on a child's development and quality of life. Understanding these effects can help in planning appropriate interventions.
- Children with PVL may have learning disabilities.
- Behavioral issues are common in children with PVL.
- Vision problems can occur due to PVL.
- Hearing impairments are also possible.
- Some children may develop epilepsy.
Preventive Measures
While not all cases of PVL can be prevented, certain measures can reduce the risk. These steps are particularly important for high-risk pregnancies.
- Regular prenatal care can help in early detection of risk factors.
- Managing maternal infections during pregnancy is crucial.
- Avoiding smoking and alcohol during pregnancy can reduce the risk.
- Proper nutrition and hydration are essential for maternal health.
- Early delivery should be avoided unless medically necessary.
Research and Future Directions
Ongoing research aims to better understand PVL and develop new treatments. Advances in medical science offer hope for improved outcomes.
- Stem cell therapy is being explored as a potential treatment for PVL.
- Research is ongoing to find neuroprotective agents that can prevent brain injury.
- Advances in neonatal care have reduced the incidence of PVL.
- Genetic studies are being conducted to understand susceptibility to PVL.
- Early intervention programs are being developed to improve outcomes.
Support and Resources
Families dealing with PVL need support and resources to navigate the challenges. Various organizations and programs offer assistance.
- The Cerebral Palsy Foundation provides resources for families.
- March of Dimes offers support for premature infants and their families.
- Early intervention programs are available in many communities.
- Support groups can help families connect with others facing similar challenges.
- Online forums and communities offer a platform for sharing experiences.
Personal Stories and Experiences
Hearing from families who have dealt with PVL can provide valuable insights and hope. Personal stories highlight the resilience and strength of these families.
- Many families share their PVL journeys on social media.
- Blogs and websites often feature personal stories about living with PVL.
- Some parents write books about their experiences with PVL.
- Documentaries and films sometimes cover the topic of PVL.
- Personal stories can inspire and offer practical advice to others.
Advocacy and Awareness
Raising awareness about PVL is crucial for early diagnosis and better support. Advocacy efforts can make a significant difference.
- World Prematurity Day raises awareness about issues like PVL.
- Advocacy groups work to improve neonatal care standards.
- Fundraising events support research and resources for PVL.
- Public awareness campaigns educate about the risks and symptoms of PVL.
- Increased awareness can lead to better funding for research and support programs.
Final Thoughts on Periventricular Leukomalacia
Periventricular Leukomalacia (PVL) is a serious condition affecting the brain's white matter, often seen in premature infants. Understanding PVL's causes, symptoms, and treatments can help caregivers and medical professionals provide better care. Early detection and intervention are crucial for improving outcomes. While PVL can lead to long-term challenges like cerebral palsy or developmental delays, advancements in neonatal care offer hope. Families dealing with PVL need support and resources to navigate this complex condition. Awareness and education about PVL can make a significant difference in the lives of affected children and their families. Stay informed, seek medical advice, and connect with support groups to manage PVL effectively. Knowledge is power when dealing with such a challenging diagnosis.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
