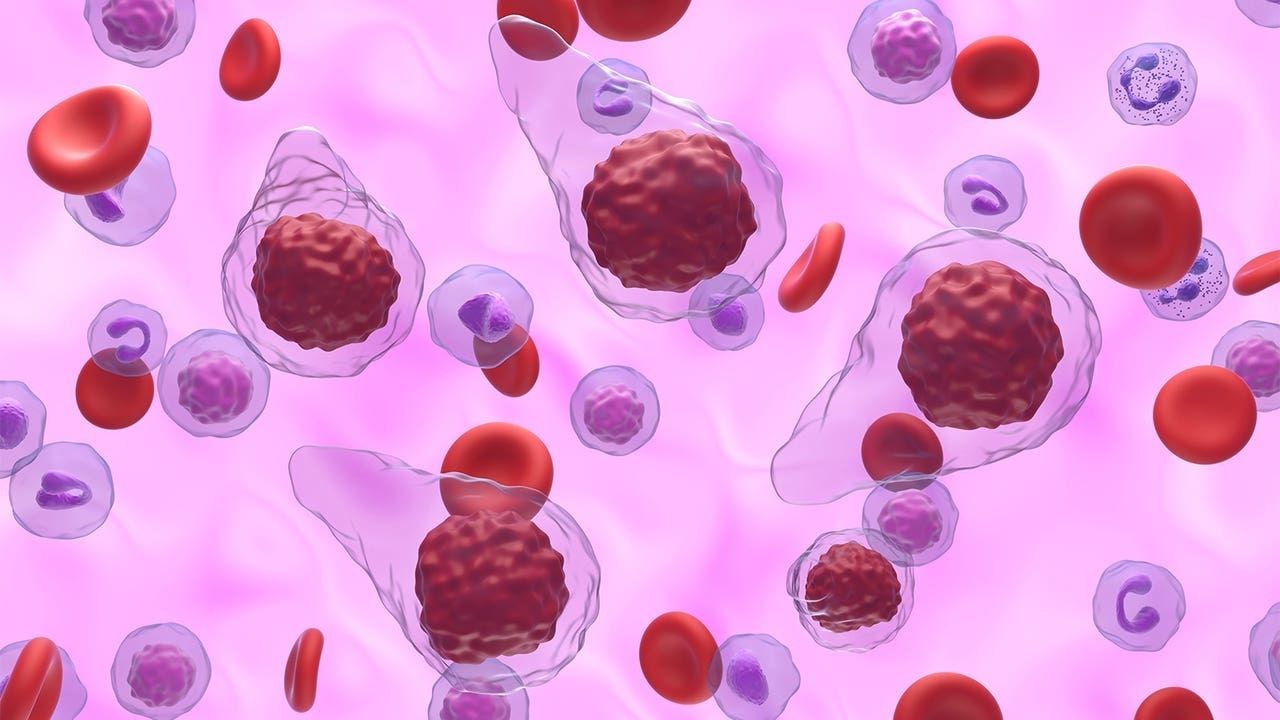
Myelofibrosis is a rare type of bone marrow cancer that disrupts the body's ability to produce blood cells. This condition leads to extensive scarring in the bone marrow, causing severe anemia, weakness, fatigue, and often an enlarged spleen. Symptoms can vary widely, making it challenging to diagnose early. Treatment options range from medications to manage symptoms to more aggressive approaches like stem cell transplants. Understanding myelofibrosis is crucial for patients and caregivers alike. This post will provide 50 essential facts about myelofibrosis, offering insights into its causes, symptoms, treatments, and ongoing research. Whether you're newly diagnosed or seeking more information, these facts will help you navigate this complex condition.
Key Takeaways:
- Myelofibrosis is a rare bone marrow cancer causing severe anemia and fatigue. Treatment options include medication, transfusions, and lifestyle adjustments for improved quality of life.
- Ongoing research aims to develop better treatments for myelofibrosis, including new medications with fewer side effects and personalized medicine approaches. Increased funding and awareness are crucial for progress.
What is Myelofibrosis?
Myelofibrosis is a rare type of bone marrow cancer that disrupts the body's normal production of blood cells. This condition leads to extensive scarring in the bone marrow, causing severe anemia, weakness, and fatigue. Let's dive into some fascinating facts about this complex disease.
- Myelofibrosis is a type of chronic leukemia that affects the bone marrow.
- It is classified as a myeloproliferative disorder, which means it involves the overproduction of blood cells.
- The disease can develop on its own (primary myelofibrosis) or as a progression of other bone marrow disorders (secondary myelofibrosis).
- Symptoms often include fatigue, night sweats, fever, and weight loss.
- An enlarged spleen, known as splenomegaly, is a common symptom due to the spleen compensating for the bone marrow's failure.
- Myelofibrosis can affect people of any age but is most commonly diagnosed in individuals over 50.
- The exact cause of myelofibrosis is unknown, though genetic mutations play a significant role.
- The JAK2 gene mutation is found in about 50-60% of myelofibrosis cases.
- Other mutations, such as CALR and MPL, are also associated with the disease.
- Myelofibrosis can lead to severe anemia, requiring frequent blood transfusions.
Diagnosis and Symptoms
Diagnosing myelofibrosis involves a combination of blood tests, bone marrow biopsies, and imaging studies. Understanding the symptoms and diagnostic process is crucial for early detection and management.
- A complete blood count (CBC) is often the first test used to detect abnormalities in blood cells.
- Bone marrow biopsy is the definitive test for diagnosing myelofibrosis.
- Imaging studies, like ultrasound or MRI, can help assess spleen and liver size.
- Symptoms can vary widely among patients, making diagnosis challenging.
- Early-stage myelofibrosis may be asymptomatic and discovered incidentally during routine blood tests.
- Advanced stages often present with more severe symptoms, including bone pain and easy bruising.
- Some patients experience pruritus, or severe itching, due to elevated levels of histamine.
- Gout, caused by high levels of uric acid, can also be a symptom.
- Myelofibrosis can lead to portal hypertension, increasing pressure in the veins of the liver.
- Patients may develop extramedullary hematopoiesis, where blood cells are produced outside the bone marrow.
Treatment Options
While there is no cure for myelofibrosis, various treatments can help manage symptoms and improve quality of life. Treatment plans are tailored to each patient's specific needs and disease progression.
- JAK inhibitors, such as ruxolitinib, are commonly used to reduce symptoms and spleen size.
- Hydroxyurea is another medication that can help control blood cell production.
- Blood transfusions are often necessary to manage anemia.
- Androgens, like danazol, can stimulate red blood cell production.
- Thalidomide and lenalidomide are used to treat anemia and reduce spleen size.
- Bone marrow or stem cell transplantation is the only potential cure but carries significant risks.
- Radiation therapy can be used to shrink an enlarged spleen.
- Splenectomy, or surgical removal of the spleen, may be considered in severe cases.
- Supportive care, including pain management and nutritional support, is essential.
- Clinical trials offer access to new and experimental treatments.
Living with Myelofibrosis
Living with myelofibrosis requires ongoing medical care and lifestyle adjustments. Patients and their families must navigate the physical and emotional challenges of the disease.
- Regular follow-up appointments are crucial for monitoring disease progression.
- Patients should maintain a healthy diet to support overall well-being.
- Exercise, tailored to individual capabilities, can help manage fatigue and improve mood.
- Support groups and counseling can provide emotional support and coping strategies.
- Patients should avoid infections by practicing good hygiene and staying up-to-date on vaccinations.
- Managing stress through relaxation techniques, like meditation or yoga, can be beneficial.
- Palliative care focuses on improving quality of life and managing symptoms.
- Advanced care planning, including discussing end-of-life wishes, is important.
- Patients may experience financial challenges due to medical costs and loss of income.
- Advocacy and awareness efforts can help improve resources and support for those affected by myelofibrosis.
Research and Future Directions
Ongoing research aims to better understand myelofibrosis and develop more effective treatments. Advances in genetics and molecular biology hold promise for the future.
- Researchers are exploring new JAK inhibitors with fewer side effects.
- Gene therapy is being investigated as a potential treatment option.
- Studies are examining the role of the immune system in myelofibrosis.
- Biomarkers are being identified to help predict disease progression and treatment response.
- Combination therapies, using multiple drugs, are being tested for improved outcomes.
- Patient registries and databases are helping to collect valuable data on the disease.
- International collaborations are accelerating research efforts.
- Advances in imaging technology are improving diagnostic accuracy.
- Personalized medicine approaches are being developed to tailor treatments to individual patients.
- Increased funding and awareness are essential for continued progress in myelofibrosis research.
Understanding Myelofibrosis
Myelofibrosis, a rare bone marrow disorder, disrupts normal blood cell production. This condition can lead to severe anemia, fatigue, and an enlarged spleen. Early diagnosis and treatment are crucial for managing symptoms and improving quality of life. Treatments range from medications to stem cell transplants, depending on the severity and progression of the disease.
Staying informed about myelofibrosis helps patients and their families navigate the challenges it presents. Regular check-ups, a healthy lifestyle, and support from healthcare professionals play vital roles in managing this condition. Awareness and education about myelofibrosis can lead to better outcomes and support for those affected.
By understanding the facts about myelofibrosis, individuals can take proactive steps in their healthcare journey. Knowledge empowers patients to make informed decisions and seek the best possible care. Stay vigilant, stay informed, and prioritize your health.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
