Microscopic Polyangiitis (MPA) is a rare autoimmune disease that affects small blood vessels, causing inflammation and damage. What makes MPA unique? Unlike other vasculitis diseases, MPA doesn't usually cause granulomas, which are clumps of immune cells. This condition can impact various organs, including the kidneys, lungs, skin, and nerves. How does it manifest? Symptoms often include fatigue, fever, weight loss, and muscle pain. Why is early diagnosis crucial? Early detection and treatment can prevent severe organ damage and improve quality of life. What treatments are available? Common treatments involve immunosuppressive medications like corticosteroids and cyclophosphamide. Want to know more? Keep reading to uncover 50 intriguing facts about MPA that will deepen your understanding of this complex disease.
Key Takeaways:
- Microscopic Polyangiitis (MPA) is a rare autoimmune disease that can affect various organs, causing symptoms like fever, weight loss, and kidney inflammation. Early diagnosis and treatment are crucial for managing the condition.
- Treatment for MPA involves medications to reduce inflammation and control the immune system, along with regular monitoring and lifestyle adjustments. Ongoing research aims to improve diagnosis and develop more effective treatments.
What is Microscopic Polyangiitis?
Microscopic Polyangiitis (MPA) is a rare autoimmune disease that causes inflammation of small blood vessels. This condition can affect various organs, leading to a wide range of symptoms. Here are some intriguing facts about MPA.
- MPA is classified under a group of diseases known as vasculitis.
- The exact cause of MPA remains unknown.
- MPA primarily affects small blood vessels, including capillaries, venules, and arterioles.
- It can lead to organ damage, particularly in the kidneys and lungs.
- MPA is more common in adults than in children.
- Symptoms can vary widely, making diagnosis challenging.
- Common symptoms include fever, weight loss, and fatigue.
- Kidney involvement can lead to glomerulonephritis, a type of kidney inflammation.
- Lung involvement may cause coughing, shortness of breath, and hemoptysis (coughing up blood).
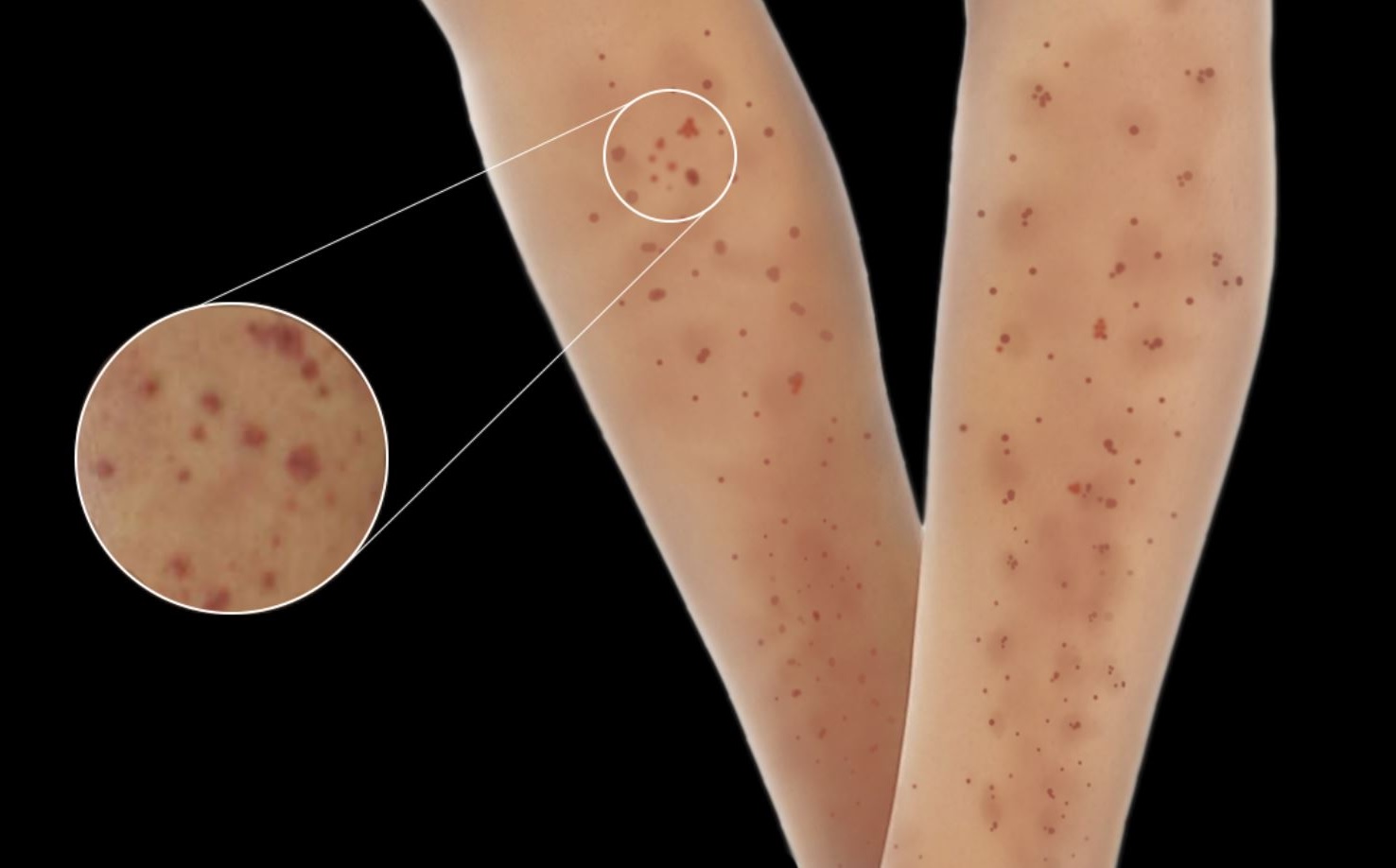
- Skin manifestations can include purpura, which are small purple spots caused by bleeding under the skin.
How is MPA Diagnosed?
Diagnosing MPA involves a combination of clinical evaluation, laboratory tests, and imaging studies. Here are some key facts about the diagnostic process.
- Blood tests can detect elevated levels of certain antibodies, such as ANCA (anti-neutrophil cytoplasmic antibodies).
- A biopsy of affected tissue can confirm the diagnosis by showing inflammation of small blood vessels.
- Urinalysis can reveal abnormalities indicating kidney involvement.
- Imaging studies like chest X-rays or CT scans can detect lung involvement.
- Early diagnosis is crucial for preventing severe organ damage.
- MPA can be mistaken for other types of vasculitis, making accurate diagnosis essential.
- Rheumatologists often play a key role in diagnosing and managing MPA.
- Genetic factors may contribute to the development of MPA, though more research is needed.
- Environmental triggers, such as infections, might play a role in triggering the disease.
- MPA is considered a chronic condition, requiring long-term management.
Treatment Options for MPA
Treatment for MPA aims to reduce inflammation, control symptoms, and prevent organ damage. Here are some important facts about treatment options.
- Corticosteroids are commonly used to reduce inflammation.
- Immunosuppressive drugs, such as cyclophosphamide or rituximab, can help control the immune system.
- Plasmapheresis, a procedure that filters the blood, may be used in severe cases.
- Maintenance therapy is often required to prevent relapses.
- Regular monitoring is essential to assess treatment effectiveness and detect potential side effects.
- Early treatment can improve the prognosis for individuals with MPA.
- Some patients may achieve remission, where symptoms are minimal or absent.
- Relapses can occur, necessitating adjustments in treatment.
- Supportive care, including managing symptoms and complications, is crucial.
- Patients with MPA often work closely with a multidisciplinary team of healthcare providers.
Living with MPA
Living with MPA can be challenging, but understanding the condition and its management can help improve quality of life. Here are some facts about living with MPA.
- Regular follow-up appointments are important for monitoring the disease.
- Patients may need to make lifestyle adjustments to manage symptoms and treatment side effects.
- A balanced diet and regular exercise can help maintain overall health.
- Stress management techniques, such as meditation or yoga, can be beneficial.
- Support groups and counseling can provide emotional support.
- Patients should avoid smoking and limit alcohol consumption.
- Vaccinations can help prevent infections, which can trigger disease flares.
- Sun protection is important, as some medications can increase sensitivity to sunlight.
- Patients should inform their healthcare providers about all medications and supplements they are taking.
- Open communication with healthcare providers is essential for effective disease management.
Research and Future Directions
Ongoing research aims to better understand MPA and develop more effective treatments. Here are some exciting facts about current research and future directions.
- Researchers are investigating the genetic basis of MPA.
- New biomarkers are being studied to improve diagnosis and monitoring.
- Advances in imaging techniques may enhance the detection of organ involvement.
- Clinical trials are testing new medications and treatment strategies.
- Personalized medicine approaches are being explored to tailor treatment to individual patients.
- Improved understanding of the immune system may lead to novel therapies.
- International collaborations are advancing research efforts.
- Patient registries are helping to collect valuable data on MPA.
- Increased awareness and education about MPA can improve early diagnosis and treatment.
- Continued research holds the promise of better outcomes for individuals with MPA.
Final Thoughts on Microscopic Polyangiitis
Microscopic Polyangiitis (MPA) is a rare but serious autoimmune disease. It primarily affects small blood vessels, leading to inflammation and damage in organs like the kidneys, lungs, and skin. Early diagnosis and treatment are crucial for managing symptoms and preventing severe complications. Treatments often include immunosuppressive medications and corticosteroids to reduce inflammation and control the immune system's overactivity.
Understanding MPA's symptoms, such as fatigue, weight loss, and muscle pain, can help in seeking timely medical advice. Regular check-ups and monitoring are essential for those diagnosed with MPA to manage the disease effectively. While living with MPA can be challenging, advancements in medical research continue to improve treatment options and quality of life for patients.
Stay informed, consult healthcare professionals, and support ongoing research to better understand and combat this complex condition.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
