Hereditary Spherocytic Hemolytic Anemia is a mouthful, right? But what exactly is it? It's a genetic disorder affecting red blood cells, causing them to become sphere-shaped instead of the usual disc shape. This change makes them more fragile and prone to breaking down, leading to anemia. Symptoms can range from mild to severe and include fatigue, jaundice, and an enlarged spleen. Diagnosing this condition often involves blood tests and family history. Treatment may include folic acid supplements, blood transfusions, or even spleen removal in severe cases. Ready to dive into 40 intriguing facts about this condition? Let's get started!
Key Takeaways:
- Hereditary Spherocytic Hemolytic Anemia (HSHA) is a genetic disorder affecting red blood cells, causing symptoms like fatigue and jaundice. It can be managed with treatments like blood transfusions and splenectomy.
- HSHA is inherited and can affect anyone, but it's more common in people of Northern European descent. Understanding its genetic basis and managing symptoms through treatments and lifestyle adjustments are crucial for individuals with HSHA.
What is Hereditary Spherocytic Hemolytic Anemia?
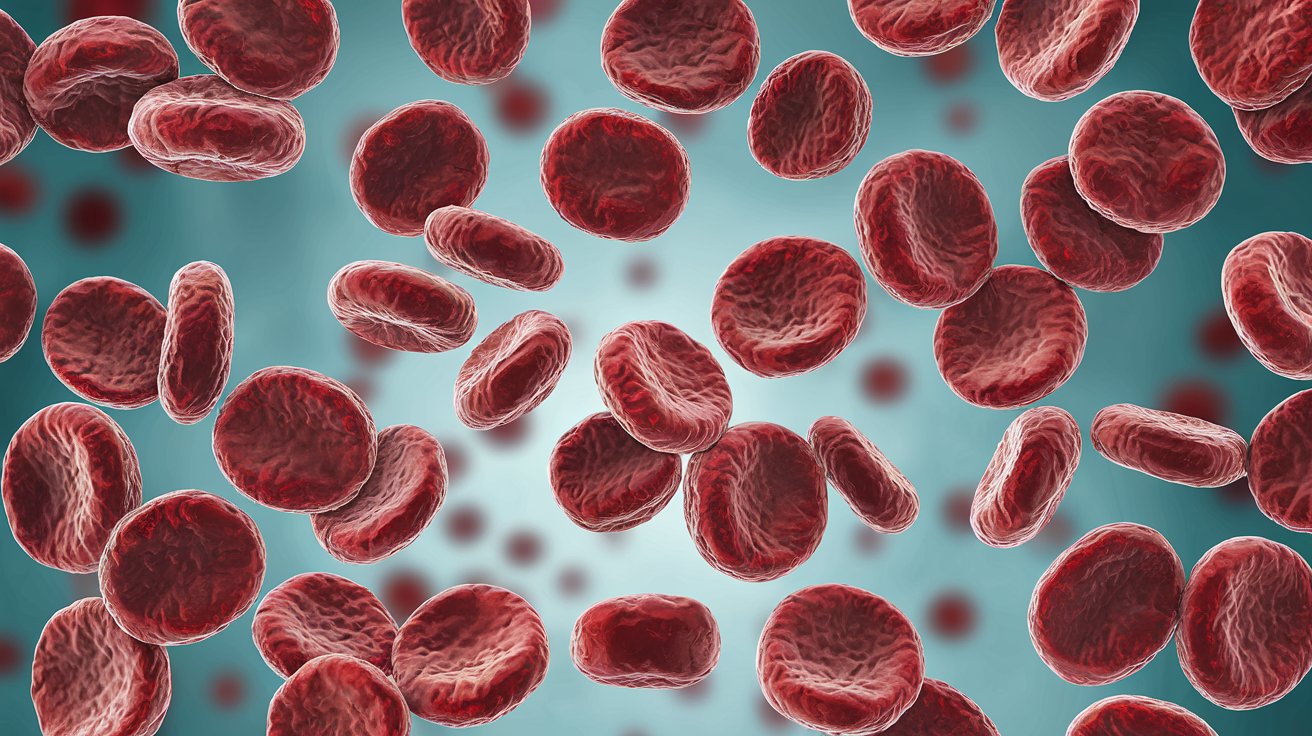
Hereditary Spherocytic Hemolytic Anemia (HSHA) is a genetic disorder affecting red blood cells. It causes these cells to become spherical and fragile, leading to their premature destruction. Here are some intriguing facts about this condition:
- HSHA is an inherited condition, meaning it is passed down from parents to children through genes.
- The disorder affects the red blood cell membrane, making the cells less flexible and more prone to breaking apart.
- Symptoms often include fatigue, jaundice, and an enlarged spleen.
- The condition is most commonly diagnosed in childhood, although it can be identified at any age.
- HSHA is more prevalent in people of Northern European descent.
- The severity of symptoms can vary widely, even among members of the same family.
- Blood tests, including a complete blood count (CBC) and a peripheral blood smear, are used to diagnose HSHA.
- The disorder can lead to complications such as gallstones and severe anemia.
- Treatment often involves managing symptoms and may include blood transfusions or removal of the spleen (splenectomy).
- Folic acid supplements are commonly recommended to help support red blood cell production.
Causes and Genetics of HSHA
Understanding the genetic basis of HSHA can shed light on why this condition occurs and how it is inherited.
- HSHA is typically caused by mutations in genes that encode proteins involved in the red blood cell membrane structure.
- The most commonly affected genes are ANK1, SPTA1, SPTB, and EPB42.
- The condition follows an autosomal dominant inheritance pattern, meaning only one copy of the mutated gene is needed to cause the disorder.
- In some cases, HSHA can also be inherited in an autosomal recessive manner, requiring two copies of the mutated gene.
- Genetic testing can confirm the presence of mutations associated with HSHA.
- Family history plays a significant role in diagnosing the condition, as it often runs in families.
- New mutations can also occur spontaneously, leading to HSHA in individuals with no family history of the disorder.
- Genetic counseling is recommended for families affected by HSHA to understand the risks and inheritance patterns.
Symptoms and Diagnosis
Recognizing the symptoms and understanding the diagnostic process is crucial for managing HSHA effectively.
- Common symptoms include pale skin, shortness of breath, and rapid heart rate due to anemia.
- Jaundice, characterized by yellowing of the skin and eyes, is a frequent symptom due to increased breakdown of red blood cells.
- An enlarged spleen (splenomegaly) occurs as the spleen works harder to remove the defective red blood cells.
- Some individuals may experience episodes of severe anemia, known as hemolytic crises.
- Blood tests reveal a high reticulocyte count, indicating increased red blood cell production to compensate for the loss.
- A peripheral blood smear shows spherocytes, which are spherical red blood cells, confirming the diagnosis.
- The osmotic fragility test measures the red blood cells' ability to withstand varying concentrations of salt solutions, helping to diagnose HSHA.
- In some cases, additional tests such as the eosin-5'-maleimide (EMA) binding test may be used for diagnosis.
Treatment and Management
Managing HSHA involves addressing symptoms and preventing complications to improve the quality of life for affected individuals.
- Regular monitoring of blood counts and overall health is essential for individuals with HSHA.
- Folic acid supplements help support the production of new red blood cells.
- Blood transfusions may be necessary during severe anemia episodes to maintain adequate red blood cell levels.
- Splenectomy, the surgical removal of the spleen, is a common treatment to reduce red blood cell destruction.
- Vaccinations against certain infections are recommended before splenectomy to prevent complications.
- After splenectomy, individuals are at increased risk of infections and may require prophylactic antibiotics.
- Gallstones, a common complication, may require surgical removal of the gallbladder.
- Iron supplements are generally avoided, as iron overload can occur due to increased red blood cell breakdown.
- Regular follow-ups with a hematologist are important for ongoing management and monitoring.
Living with HSHA
Living with HSHA requires adapting to the condition and taking steps to maintain overall health and well-being.
- A balanced diet rich in vitamins and minerals supports overall health and red blood cell production.
- Regular exercise helps improve energy levels and overall fitness.
- Avoiding activities that may cause trauma to the spleen, such as contact sports, is recommended.
- Staying hydrated is important, as dehydration can exacerbate symptoms of anemia.
- Support groups and counseling can provide emotional support and resources for individuals and families affected by HSHA.
Final Thoughts on Hereditary Spherocytic Hemolytic Anemia
Hereditary Spherocytic Hemolytic Anemia (HSHA) is a rare genetic disorder affecting red blood cells. Understanding its symptoms, causes, and treatments can help manage the condition better. Key symptoms include jaundice, anemia, and an enlarged spleen. The disorder is usually inherited from one or both parents. Diagnosis often involves blood tests and family history analysis.
Treatment options range from folic acid supplements to splenectomy, depending on severity. Regular monitoring and medical check-ups are crucial for managing HSHA effectively. Awareness and education about this condition can improve the quality of life for those affected.
By staying informed and proactive, individuals with HSHA can lead healthier lives. Always consult healthcare professionals for personalized advice and treatment plans. Knowledge is power when dealing with hereditary conditions like HSHA.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
