Stewart–Treves Syndrome is a rare but serious condition that often flies under the radar. This syndrome typically arises in individuals who have experienced chronic lymphedema, usually after cancer treatment. But what exactly is Stewart–Treves Syndrome? In simple terms, it’s a type of cancer known as angiosarcoma that develops in areas with long-standing lymphedema. Understanding this condition is crucial because early detection can significantly impact outcomes. This blog post will delve into 30 essential facts about Stewart–Treves Syndrome, shedding light on its causes, symptoms, diagnosis, and treatment options. Whether you’re a patient, caregiver, or just curious, these facts will provide valuable insights into this rare but impactful syndrome.
Key Takeaways:
- Stewart–Treves Syndrome is a rare and serious condition linked to chronic lymphedema, often occurring after cancer treatment. Early detection and proper management of lymphedema are crucial for prevention.
- Named after doctors Stewart and Treves, this syndrome involves the development of angiosarcoma, a rare and aggressive cancer. Regular medical check-ups and patient education are important for early detection and better outcomes.
What is Stewart–Treves Syndrome?
Stewart–Treves Syndrome (STS) is a rare but serious condition. It typically occurs in patients who have chronic lymphedema, often after cancer treatment. Let's dive into some fascinating facts about this syndrome.
-
Named After Doctors: The syndrome is named after Dr. Frederick Stewart and Dr. Norman Treves, who first described it in 1948.
-
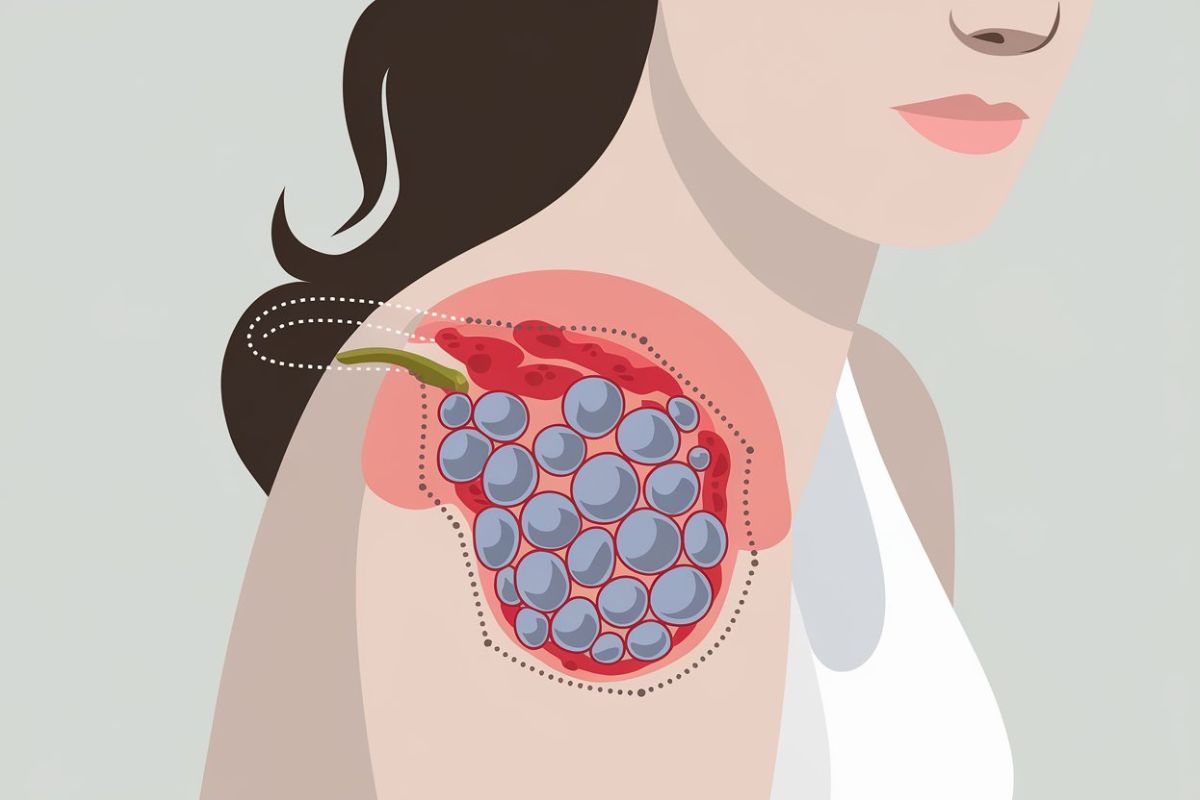
Lymphedema Link: STS usually develops in people with long-standing lymphedema, a condition where lymph fluid builds up in tissues causing swelling.
-
Cancer Connection: It often appears in patients who have had breast cancer surgery, particularly those who have undergone mastectomy and radiation therapy.
-
Angiosarcoma: The syndrome involves the development of angiosarcoma, a rare and aggressive cancer of the blood vessels.
-
Symptoms: Early signs include purple or red patches on the skin, which can be mistaken for bruises or infections.
Causes and Risk Factors
Understanding the causes and risk factors can help in early detection and prevention. Here are some key points.
-
Radiation Therapy: Radiation treatment for cancer can damage lymphatic vessels, increasing the risk of developing STS.
-
Chronic Lymphedema: Long-term lymphedema is the most significant risk factor. The longer the lymphedema persists, the higher the risk.
-
Immune System: A weakened immune system can make it easier for cancerous cells to develop in areas affected by lymphedema.
-
Genetics: While not common, genetic factors may play a role in the development of STS.
-
Age: Older individuals are more likely to develop STS, particularly those over the age of 50.
Diagnosis and Detection
Early diagnosis is crucial for better outcomes. Here’s how doctors identify Stewart–Treves Syndrome.
-
Biopsy: A skin biopsy is often performed to confirm the presence of angiosarcoma.
-
Imaging Tests: MRI and CT scans help in assessing the extent of the disease.
-
Blood Tests: While not definitive, blood tests can provide additional information about the patient’s overall health.
-
Physical Examination: Doctors look for characteristic skin changes and swelling during a physical exam.
-
Histopathology: Examining tissue samples under a microscope helps in identifying cancerous cells.
Treatment Options
Treatment for Stewart–Treves Syndrome is challenging but there are several approaches.
-
Surgery: Surgical removal of the tumor is often the first line of treatment.
-
Radiation Therapy: Post-surgical radiation can help in controlling the spread of cancer.
-
Chemotherapy: Chemotherapy may be used, especially if the cancer has spread to other parts of the body.
-
Targeted Therapy: Newer treatments focus on targeting specific cancer cells without affecting healthy cells.
-
Palliative Care: For advanced cases, palliative care focuses on relieving symptoms and improving quality of life.
Prognosis and Survival Rates
The prognosis for STS can vary. Here’s what you need to know.
-
Aggressive Nature: Angiosarcoma is highly aggressive, making early detection crucial.
-
Survival Rates: The five-year survival rate is low, often less than 20%.
-
Recurrence: Even after treatment, there is a high risk of recurrence.
-
Metastasis: The cancer can spread to other parts of the body, including the lungs and liver.
-
Follow-Up Care: Regular follow-up is essential for monitoring and managing any recurrence.
Prevention and Awareness
While prevention is difficult, awareness can lead to early detection and better outcomes.
-
Lymphedema Management: Proper management of lymphedema can reduce the risk of developing STS.
-
Regular Check-Ups: Regular medical check-ups can help in early detection of any suspicious changes.
-
Patient Education: Educating patients about the risks and symptoms of STS is crucial.
-
Support Groups: Joining support groups can provide emotional support and valuable information.
-
Research: Ongoing research is essential for developing better treatments and improving survival rates.
Final Thoughts on Stewart–Treves Syndrome
Stewart–Treves Syndrome, a rare but serious condition, often emerges in individuals with chronic lymphedema. This cancer, primarily angiosarcoma, develops in areas with long-standing swelling. Early detection and treatment are crucial for better outcomes. Regular check-ups and monitoring any changes in the skin can make a significant difference. Although rare, understanding the risks and symptoms can help in managing and potentially preventing this syndrome. If you or someone you know has chronic lymphedema, staying informed and vigilant is key. Always consult healthcare professionals for advice tailored to individual health needs. Knowledge and proactive care can go a long way in dealing with this condition. Stay aware, stay healthy.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
