Malignant Infantile Osteopetrosis is a rare genetic disorder that affects bone growth and density. Did you know that this condition can lead to bones becoming overly dense and brittle, making them prone to fractures? Children with this disorder often face challenges such as vision and hearing loss, frequent infections, and growth delays. Early diagnosis and treatment are crucial for managing symptoms and improving quality of life. Bone marrow transplants are currently the most effective treatment option. Understanding this condition can help families and caregivers provide better support and care for affected children. Here are 30 facts that will give you a deeper insight into Malignant Infantile Osteopetrosis.
Key Takeaways:
- Malignant Infantile Osteopetrosis (MIOP) is a rare genetic disorder causing dense and brittle bones. Early diagnosis and hematopoietic stem cell transplantation (HSCT) can significantly improve life expectancy and quality of life.
- MIOP, also known as Albers-Schönberg disease, affects 1 in 200,000 to 300,000 births. Understanding its genetic basis and treatment options, such as HSCT, is crucial for managing this rare condition.
What is Malignant Infantile Osteopetrosis?
Malignant Infantile Osteopetrosis (MIOP) is a rare genetic disorder affecting bone growth. This condition causes bones to become overly dense and brittle. Understanding MIOP is crucial for those affected and their families.
-
MIOP is also known as Albers-Schönberg disease. Named after the German radiologist who first described it in 1904.
-
It is an autosomal recessive disorder. Both parents must carry the gene for a child to inherit the condition.
-
MIOP affects approximately 1 in 200,000 to 300,000 births. This makes it an extremely rare condition.
-
The disorder is characterized by increased bone density. Bones become abnormally hard and brittle.
-
Symptoms usually appear within the first year of life. Early diagnosis is essential for managing the condition.
Symptoms and Diagnosis
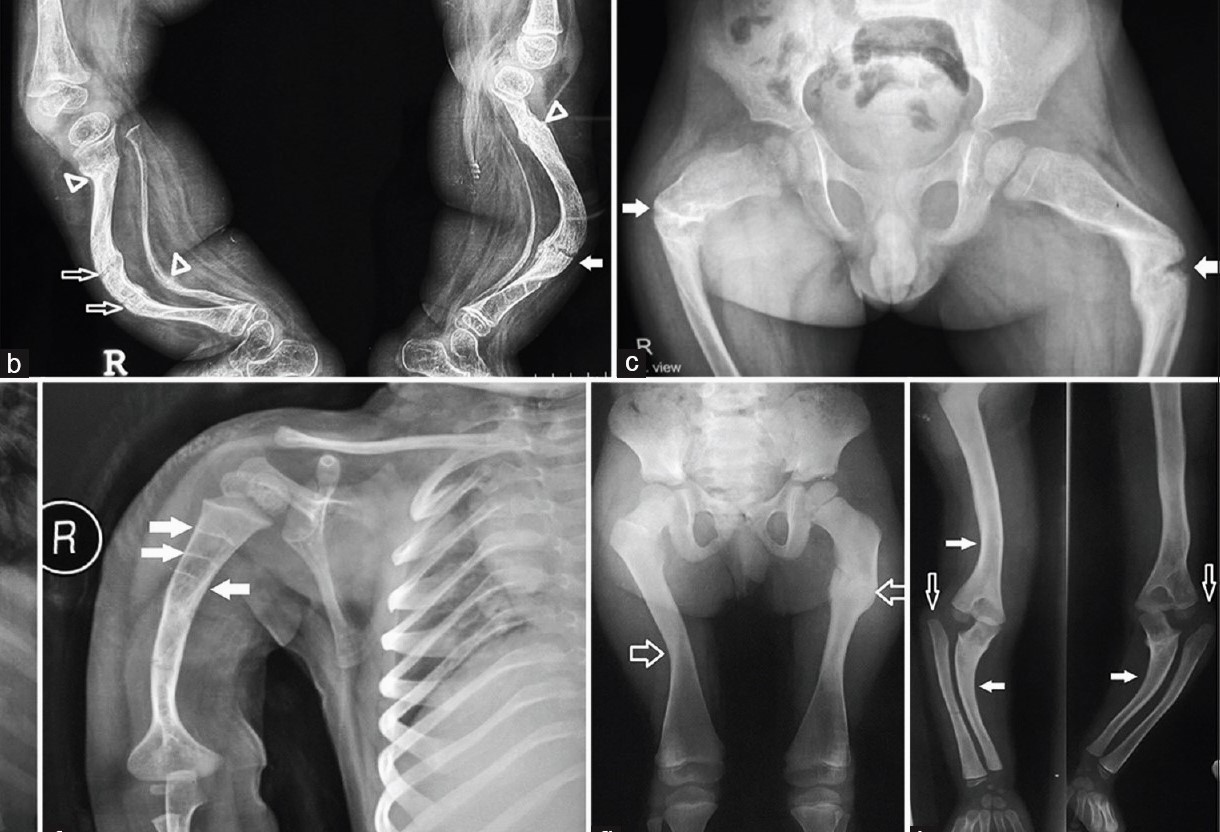
Recognizing the symptoms of MIOP can lead to early intervention. Diagnosis often involves a combination of clinical evaluation and imaging studies.
-
Common symptoms include frequent fractures. Despite increased bone density, bones are more prone to breaking.
-
Children may experience delayed growth. This can lead to short stature and other developmental issues.
-
Vision and hearing loss are possible. The dense bones can compress nerves, affecting sensory functions.
-
Anemia is a frequent complication. The bone marrow space is reduced, affecting blood cell production.
-
Diagnosis often involves X-rays. These images reveal the characteristic dense bones.
Genetic and Molecular Basis
Understanding the genetic and molecular basis of MIOP can help in developing targeted treatments. Research is ongoing to uncover the exact mechanisms.
-
Mutations in the TCIRG1 gene are a common cause. This gene is crucial for bone resorption.
-
Other genes like CLCN7 and OSTM1 can also be involved. Mutations in these genes disrupt normal bone metabolism.
-
Bone resorption is impaired in MIOP. Osteoclasts, the cells responsible for breaking down bone, do not function properly.
-
Genetic testing can confirm the diagnosis. Identifying the specific mutation helps in understanding the prognosis.
-
Carrier testing is available for at-risk families. This can help in family planning and early intervention.
Treatment Options
While there is no cure for MIOP, several treatment options can help manage symptoms and improve quality of life.
-
Hematopoietic stem cell transplantation (HSCT) is the only curative treatment. This procedure replaces the defective bone marrow with healthy cells.
-
HSCT is most effective when performed early. The best outcomes are seen in children under two years old.
-
Supportive treatments include blood transfusions. These help manage anemia and other blood-related issues.
-
Physical therapy can improve mobility. Strengthening muscles and improving coordination are key goals.
-
Surgical interventions may be necessary. Procedures to correct fractures or decompress nerves can be required.
Prognosis and Life Expectancy
The prognosis for children with MIOP varies widely. Early diagnosis and treatment can significantly improve outcomes.
-
Without treatment, MIOP can be life-threatening. Complications like severe anemia and infections are common.
-
HSCT can dramatically improve life expectancy. Many children who undergo successful transplantation live into adulthood.
-
Regular monitoring is essential. Ongoing medical care helps manage complications and improve quality of life.
-
Bone density may normalize after HSCT. This reduces the risk of fractures and other bone-related issues.
-
Early intervention is crucial for the best outcomes. Timely treatment can prevent many of the severe complications associated with MIOP.
Research and Future Directions
Ongoing research aims to improve understanding and treatment of MIOP. Advances in genetics and molecular biology hold promise for the future.
-
Gene therapy is a potential future treatment. Correcting the genetic defect at its source could provide a cure.
-
New drugs are being developed to enhance bone resorption. These could help manage symptoms without the need for transplantation.
-
Animal models are used to study MIOP. These models help researchers understand the disease and test new treatments.
-
International collaborations are crucial. Sharing knowledge and resources accelerates progress in understanding and treating MIOP.
-
Patient registries help track outcomes. Collecting data on affected individuals improves understanding of the disease and its treatment.
Final Thoughts on Malignant Infantile Osteopetrosis
Malignant Infantile Osteopetrosis (MIOP) is a rare, serious condition that affects bone growth and development in infants. Understanding MIOP can help families and caregivers better navigate the challenges it presents. Early diagnosis and treatment are crucial for improving outcomes. Bone marrow transplants offer hope, but they come with risks and require careful consideration. Genetic counseling can provide valuable insights for families with a history of the condition.
Staying informed and connected with medical professionals and support groups can make a significant difference. While MIOP is a tough journey, advancements in medical research continue to bring new possibilities for treatment and management. Remember, knowledge is power. The more you know about MIOP, the better equipped you'll be to handle its challenges. Keep advocating for research and support to improve the lives of those affected by this condition.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
