Congenital prekallikrein (PK) deficiency is a rare blood disorder that often flies under the radar. This condition affects the body's ability to produce prekallikrein, a protein crucial for blood clotting. PK deficiency can lead to prolonged bleeding times, making even minor injuries a cause for concern. Despite its rarity, understanding this condition is vital for those affected and their families. In this blog post, we'll dive into 30 intriguing facts about congenital PK deficiency, shedding light on its causes, symptoms, and management. Whether you're newly diagnosed or just curious, these facts will help you grasp the essentials of this unique medical condition.
Key Takeaways:
- Congenital Prekallikrein (PK) deficiency is a rare blood disorder that affects blood clotting. It's often asymptomatic and diagnosed incidentally, so awareness and genetic testing are crucial for effective management.
- While PK deficiency doesn't usually cause symptoms, monitoring and preventive measures may be necessary for some individuals. Ongoing research and genetic counseling offer hope for better understanding and management of this rare condition.
What is Congenital Prekallikrein (PK) Deficiency?
Congenital Prekallikrein (PK) deficiency, also known as Fletcher factor deficiency, is a rare blood disorder. It affects the body's ability to properly form blood clots. Here are some fascinating facts about this condition.
- Rare Disorder: PK deficiency is extremely rare, with only about 100 cases reported worldwide.
- Genetic Basis: This condition is inherited in an autosomal recessive manner, meaning both parents must carry the gene.
- Discovered in 1965: The disorder was first identified by Dr. Fletcher, hence the name Fletcher factor deficiency.
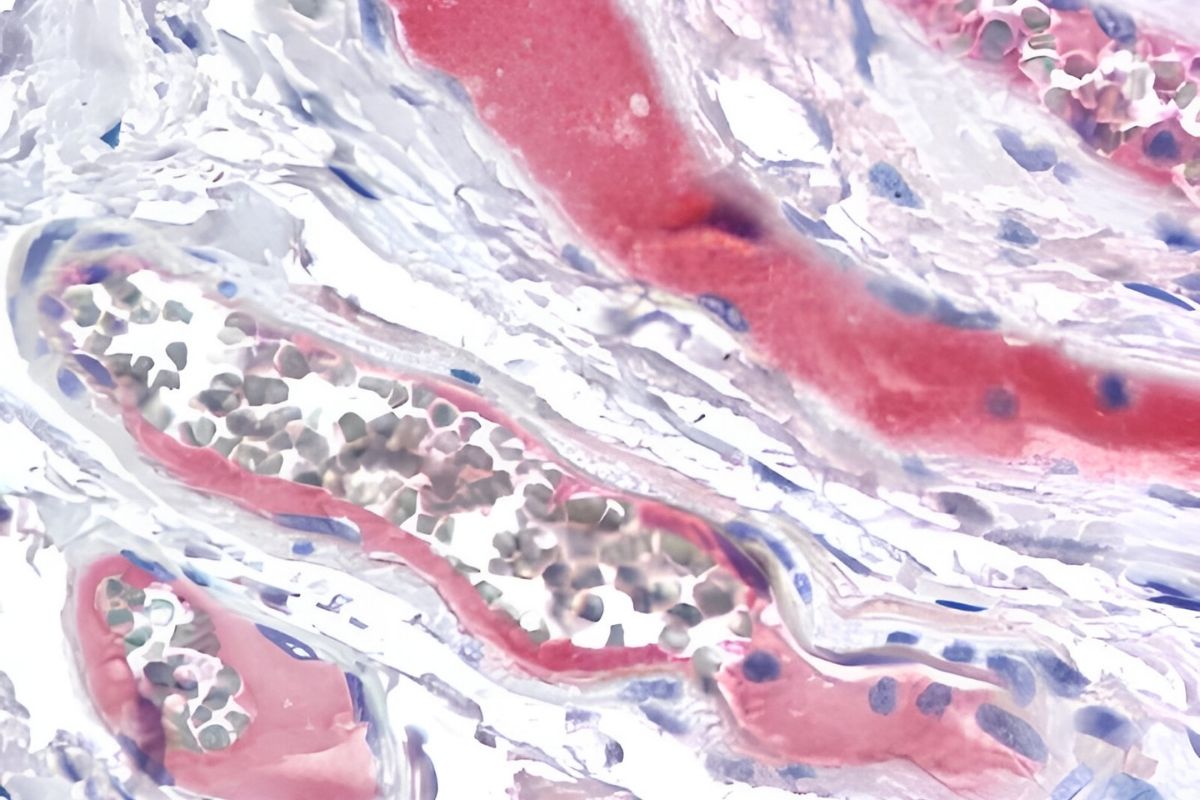
- Affects Clotting: PK deficiency impacts the intrinsic pathway of the coagulation cascade, which is crucial for blood clotting.
- No Symptoms: Many individuals with PK deficiency are asymptomatic and may never know they have it.
- Prolonged aPTT: A hallmark of PK deficiency is a prolonged activated partial thromboplastin time (aPTT) in blood tests.
- Normal PT: Despite prolonged aPTT, the prothrombin time (PT) remains normal.
- Bleeding Risk: Unlike other clotting disorders, PK deficiency does not typically increase the risk of bleeding.
- Thrombosis Risk: Some studies suggest a potential increased risk of thrombosis, though this is not well-established.
- Diagnosis: Diagnosis often occurs incidentally during routine blood tests or pre-surgical screenings.
Symptoms and Diagnosis
Understanding the symptoms and diagnostic methods is crucial for managing PK deficiency. Here are some key points.
- Asymptomatic Nature: Most people with PK deficiency show no symptoms.
- Incidental Finding: The condition is often discovered accidentally during blood tests for other reasons.
- Family History: A family history of PK deficiency can prompt testing in relatives.
- Specialized Tests: Specific blood tests, including aPTT and PK activity assays, are used for diagnosis.
- Differential Diagnosis: PK deficiency must be differentiated from other clotting disorders like hemophilia.
- Genetic Testing: Genetic testing can confirm the presence of mutations in the KLKB1 gene, responsible for PK deficiency.
- Prenatal Testing: In families with a known history, prenatal testing can identify PK deficiency in the fetus.
- No Routine Screening: Routine screening for PK deficiency is not recommended due to its rarity and asymptomatic nature.
Treatment and Management
Managing PK deficiency involves understanding treatment options and lifestyle adjustments. Here are some important facts.
- No Specific Treatment: There is no specific treatment for PK deficiency since it usually doesn't cause symptoms.
- Monitoring: Regular monitoring of blood clotting parameters may be recommended for some individuals.
- Preventive Measures: In cases with a history of thrombosis, preventive measures like anticoagulants may be considered.
- Surgical Precautions: Special precautions are taken during surgeries to manage potential clotting issues.
- Avoiding Risk Factors: Individuals are advised to avoid risk factors for thrombosis, such as smoking and prolonged immobility.
- Education: Educating patients and families about the condition is crucial for effective management.
- Genetic Counseling: Genetic counseling can help families understand the inheritance pattern and risks.
Research and Future Directions
Ongoing research aims to better understand PK deficiency and improve management strategies. Here are some insights.
- Research Gaps: There are still many unknowns about the clinical significance of PK deficiency.
- Thrombosis Link: More research is needed to clarify the potential link between PK deficiency and thrombosis.
- Gene Therapy: Advances in gene therapy may offer future treatment options for genetic disorders like PK deficiency.
- Clinical Trials: Participation in clinical trials can help advance understanding and treatment of PK deficiency.
- Awareness: Increasing awareness among healthcare providers can lead to better diagnosis and management of this rare condition.
Understanding PK Deficiency
PK deficiency, though rare, plays a significant role in understanding blood clotting disorders. Knowing the symptoms and diagnosis methods can help in early detection and management. This condition often goes unnoticed due to its mild or asymptomatic nature, making awareness crucial. Genetic testing and family history are key in identifying those at risk.
Treatment options, while limited, focus on managing symptoms and preventing complications. Regular check-ups and consultations with a hematologist can make a big difference in patient outcomes. Staying informed about the latest research and advancements in treatment can also provide hope for those affected.
By spreading knowledge about PK deficiency, we can support those living with this condition and contribute to ongoing research efforts. Remember, awareness and education are the first steps toward better health and improved quality of life for everyone.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
