Pancreatic neuroendocrine tumors, often called islet cell tumors, are rare growths that start in the hormone-producing cells of the pancreas. These tumors can be either benign or malignant, but they are distinct from the more common pancreatic adenocarcinoma. What makes these tumors unique? They can produce hormones like insulin, gastrin, or glucagon, leading to various symptoms depending on the type of hormone released. Some people might experience low blood sugar, stomach ulcers, or skin rashes. Why should you care? Understanding these tumors is crucial because early detection can significantly impact treatment options and outcomes. While they account for a small percentage of pancreatic cancers, their potential to disrupt hormone balance makes them noteworthy. Want to know more? We’ll explore 25 intriguing facts about these tumors, shedding light on their characteristics, symptoms, and treatment options. Stay tuned to learn how these rare tumors can affect the body and what can be done about them.
Key Takeaways:
- Pancreatic neuroendocrine tumors (PNETs) are rare and can produce hormones, causing varied symptoms. Early detection and treatment are crucial for better prognosis and survival rates.
- Living with PNETs involves managing symptoms, regular monitoring, balanced diet, support systems, and hope for new treatments through research and clinical trials.
Understanding Pancreatic Neuroendocrine Tumors
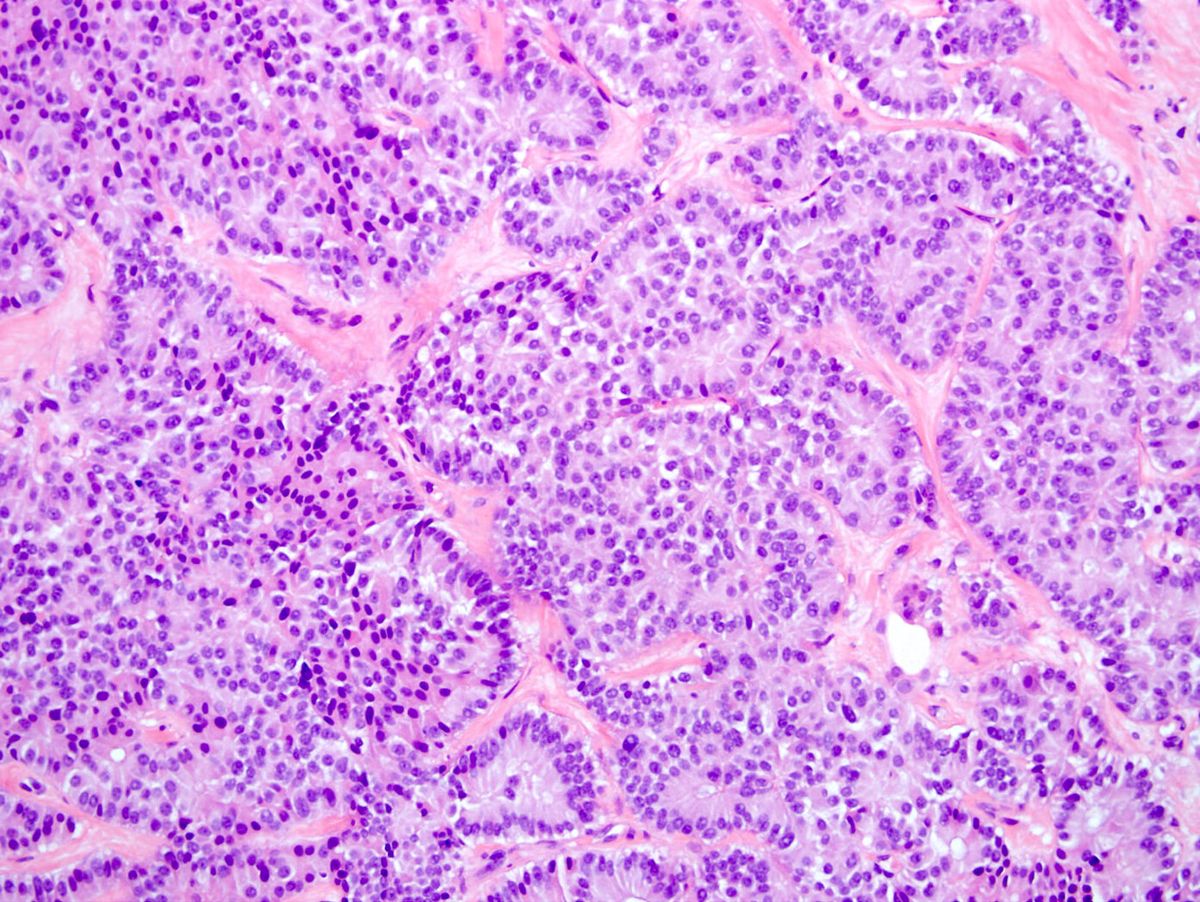
Pancreatic neuroendocrine tumors (PNETs), also known as islet cell tumors, are a rare type of cancer that forms in the hormone-producing cells of the pancreas. These tumors can be benign or malignant and often have unique characteristics compared to other pancreatic cancers.
-
Rare Occurrence: PNETs make up only about 1-2% of all pancreatic cancers, making them quite rare.
-
Hormone Production: Unlike other pancreatic tumors, PNETs can produce hormones, leading to various symptoms depending on the hormone released.
-
Types of PNETs: There are several types, including insulinomas, gastrinomas, glucagonomas, and VIPomas, each named after the hormone they produce.
-
Slow Growth: Many PNETs grow slowly, which can sometimes delay diagnosis as symptoms develop gradually.
-
Genetic Links: Some PNETs are linked to genetic conditions like Multiple Endocrine Neoplasia type 1 (MEN1).
Symptoms and Diagnosis
Symptoms of PNETs can vary widely, often depending on the type of hormone the tumor secretes. Diagnosis can be challenging due to the rarity and varied presentation of these tumors.
-
Varied Symptoms: Symptoms can range from abdominal pain and weight loss to more specific signs like hypoglycemia in insulinomas.
-
Imaging Tests: CT scans, MRIs, and PET scans are commonly used to locate and assess PNETs.
-
Biopsy for Confirmation: A biopsy is often necessary to confirm the diagnosis and determine the tumor type.
-
Blood Tests: Hormone levels in the blood can provide clues to the presence of a PNET.
-
Endoscopic Ultrasound: This procedure can help visualize the tumor and guide biopsy.
Treatment Options
Treatment for PNETs depends on the type, size, and spread of the tumor. Options range from surgery to medication.
-
Surgical Removal: Surgery is often the primary treatment for localized PNETs.
-
Medication: Drugs like somatostatin analogs can help control hormone-related symptoms.
-
Targeted Therapy: Everolimus and sunitinib are examples of targeted therapies used for advanced PNETs.
-
Chemotherapy: Used less frequently, chemotherapy may be an option for aggressive or widespread tumors.
-
Radiation Therapy: In some cases, radiation may be used to shrink tumors or relieve symptoms.
Prognosis and Survival Rates
The outlook for individuals with PNETs can vary significantly based on several factors, including tumor type and stage at diagnosis.
-
Better Prognosis: PNETs generally have a better prognosis than other types of pancreatic cancer.
-
Survival Rates: The five-year survival rate for localized PNETs can be as high as 90%.
-
Influence of Tumor Type: Functional tumors, which produce hormones, may have different outcomes compared to non-functional ones.
-
Importance of Early Detection: Early detection and treatment significantly improve survival chances.
-
Role of Genetics: Genetic testing can provide insights into prognosis and guide treatment decisions.
Living with PNETs
Living with PNETs involves managing symptoms, treatment side effects, and maintaining quality of life.
-
Symptom Management: Hormone-related symptoms can often be managed with medication.
-
Regular Monitoring: Regular follow-up appointments are crucial for monitoring tumor growth and treatment effectiveness.
-
Diet and Nutrition: A balanced diet can help manage symptoms and improve overall health.
-
Support Systems: Support groups and counseling can be beneficial for emotional and mental well-being.
-
Research and Clinical Trials: Ongoing research and clinical trials offer hope for new treatments and improved outcomes.
Final Thoughts on Pancreatic Neuroendocrine Tumors
Pancreatic neuroendocrine tumors (PNETs), also known as islet cell tumors, are rare but significant. Understanding these tumors is crucial for early detection and treatment. They arise from the hormone-producing cells in the pancreas and can be either benign or malignant. Symptoms vary widely, often depending on whether the tumor is functioning or non-functioning. Functioning tumors secrete hormones, leading to symptoms like hypoglycemia or gastrinoma, while non-functioning ones might not show symptoms until they grow large.
Diagnosis typically involves imaging tests and blood work, sometimes followed by a biopsy. Treatment options range from surgery to medication, depending on the tumor's type and stage. Research continues to advance, offering hope for better outcomes. Staying informed and consulting healthcare professionals can make a big difference in managing this condition. Awareness and early intervention remain key in tackling PNETs effectively.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
