Tumor immunology is a rapidly evolving field that explores the complex relationship between the immune system and cancer. In recent years, there have been remarkable advancements in our understanding of how the immune system interacts with tumors, leading to the development of novel immunotherapies that have revolutionized cancer treatment.
In this article, we’ll delve into the fascinating world of tumor immunology and uncover 18 intriguing facts that will not only deepen your knowledge but also ignite your curiosity about this groundbreaking field. From the role of T cells and natural killer cells in tumor surveillance to the mechanisms of immune evasion employed by cancer cells, these facts will shed light on the intricate battle between the immune system and cancer.
So, if you’re ready to embark on a journey through the captivating world of tumor immunology, let’s dive in and discover some astonishing facts that highlight the power and potential of harnessing the immune system to fight cancer.
Key Takeaways:
- The immune system can be trained to fight cancer through immunotherapy, offering hope for more effective and targeted cancer treatments.
- Understanding how the immune system interacts with cancer cells can lead to innovative therapies, such as CAR-T cell and gut microbiome-based treatments, improving cancer care.
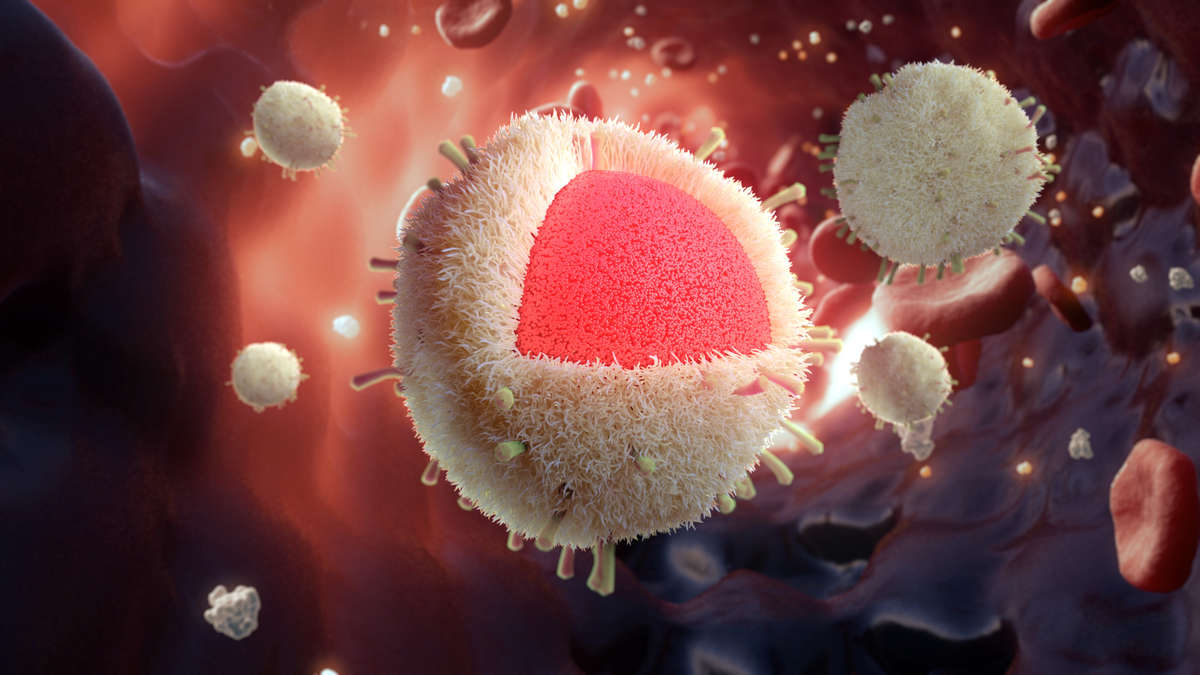
Tumor Immunology is a branch of immunology that focuses on the interaction between the immune system and cancer cells.
Tumor immunology explores how the immune system can recognize and eliminate cancer cells or how cancer cells can evade immune surveillance.
Immunotherapy, a treatment approach that utilizes the body’s immune system to fight against cancer, is a major field in tumor immunology.
Immunotherapy has revolutionized cancer treatment by harnessing the power of the immune system to specifically target and destroy cancer cells.
Checkpoint inhibitors are a type of immunotherapy that blocks the proteins on cancer cells, allowing immune cells to recognize and attack them.
Checkpoint inhibitors have shown remarkable efficacy in treating various types of cancer and have significantly improved patient outcomes.
Tumor-infiltrating lymphocytes (TILs) are a type of immune cells that infiltrate the tumor microenvironment and play a critical role in tumor defense.
TILs can recognize and selectively kill cancer cells, but their function can be suppressed by various mechanisms employed by tumors.
Cancer cells can evade the immune system through mechanisms such as downregulating the expression of major histocompatibility complex (MHC) molecules.
This allows cancer cells to escape recognition by immune cells and avoid being targeted for destruction.
Dendritic cells are professional antigen-presenting cells that play a crucial role in initiating immune responses against cancer cells.
Dendritic cells capture and present tumor antigens to immune cells, triggering an immune response specifically targeting the cancer cells.
Cancer vaccines aim to stimulate the immune system to recognize and attack cancer cells by presenting them with cancer-specific antigens.
These vaccines can be based on tumor antigens, dendritic cells, or genetic materials encoding tumor-specific proteins.
The tumor microenvironment consists of various cell types, including immune cells, fibroblasts, and blood vessels, which interact with cancer cells.
These interactions can either promote or inhibit tumor growth and metastasis, depending on the specific cellular and molecular signals involved.
Chimeric antigen receptor (CAR) T-cell therapy is an innovative immunotherapy approach that involves modifying a patient’s T cells to express synthetic receptors.
These receptors enable the T cells to recognize and target cancer cells expressing specific antigens, leading to their destruction.
Tumor-associated antigens (TAAs) are molecules expressed by cancer cells that can be specifically recognized by the immune system.
TAAs are often overexpressed or mutated in cancer cells, making them attractive targets for immunotherapy.
T regulatory cells (Tregs) are a subset of immune cells that can suppress immune responses, including those against cancer cells.
High levels of Tregs in the tumor microenvironment can create an immunosuppressive environment that hinders the effectiveness of immunotherapies.
Cancer immunotherapy can cause immune-related adverse events (irAEs), which are side effects resulting from the activation of the immune system.
These side effects can affect various organs and systems and require close monitoring and management during cancer treatment.
The gut microbiome, the collection of microorganisms residing in the digestive tract, can influence the response to cancer immunotherapy.
Specific bacteria in the gut microbiome have been shown to enhance or inhibit the effectiveness of immunotherapy treatments.
Tumor-infiltrating lymphocytes (TILs) can be isolated from tumors, expanded in the laboratory, and infused back into patients as a form of adoptive cell therapy.
This approach has shown promising results in the treatment of certain types of cancer, particularly melanoma.
Tumor-associated macrophages (TAMs) are immune cells that infiltrate the tumor microenvironment and can have either pro-tumor or anti-tumor effects.
The polarization of TAMs towards an anti-tumor phenotype is a potential target for immunotherapy strategies.
Combination therapies that involve the simultaneous or sequential use of different immunotherapeutic agents are being explored to enhance treatment outcomes.
These combinations can target different aspects of the immune response to maximize the anti-cancer effects.
Immunosurveillance is a process by which the immune system constantly monitors and eliminates cancer cells before they develop into clinically detectable tumors.
Understanding the mechanisms of immunoediting can provide insights into developing strategies to boost immunosurveillance.
CAR-NK (natural killer) cell therapy is an emerging approach that utilizes engineered natural killer cells to target and kill cancer cells.
This therapy holds promise for the treatment of hematological malignancies and solid tumors.
Conclusion
Understanding tumor immunology is crucial in advancing our knowledge and treatment options for cancer. The intricate relationship between tumors and the immune system has paved the way for groundbreaking discoveries and therapies. From the identification of cancer cells by immune cells to the development of immunotherapies, tumor immunology continues to be an exciting and evolving field.
By harnessing the power of the immune system, scientists and researchers are able to enhance the body’s ability to recognize and destroy cancer cells. This has led to significant advancements in cancer treatment, with immunotherapies showing promising results in various types of cancer.
As our understanding of tumor immunology continues to grow, we can expect even more innovative approaches to cancer treatment that are targeted, effective, and have fewer side effects. Through ongoing research and collaboration, we are moving closer to a future where cancer can be effectively managed, if not eradicated, thanks to the fascinating world of tumor immunology.
FAQs
1. What is tumor immunology?
Tumor immunology is the study of the interactions between the immune system and cancer cells. It explores how the immune system recognizes and targets cancer cells, as well as the mechanisms cancer cells use to evade immune detection.
2. What are immunotherapies?
Immunotherapies are treatments that harness the power of the immune system to fight cancer. They work by stimulating the immune system, enhancing its ability to recognize and destroy cancer cells.
3. How do immunotherapies work?
Immunotherapies work by targeting specific components of the immune system or cancer cells. They can either boost the immune response, prevent cancer cells from evading immune detection, or directly attack the cancer cells.
4. What are some examples of immunotherapies?
Examples of immunotherapies include immune checkpoint inhibitors, CAR-T cell therapy, therapeutic vaccines, and cytokines.
5. Are immunotherapies effective for all types of cancer?
No, the effectiveness of immunotherapy varies depending on the type of cancer and individual patient factors. Some cancers have shown remarkable responses to immunotherapies, while others may be less responsive.
6. What are the potential side effects of immunotherapy?
Although immunotherapies are generally well-tolerated, they can cause side effects. These can range from mild symptoms like fatigue and rash to more severe immune-related adverse events, which may require medical intervention.
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
