Milwaukee Shoulder Syndrome might sound like a rare condition, but it's more common than you think. This painful disorder primarily affects older adults, especially women. Characterized by the rapid destruction of shoulder joints, it can lead to severe pain and limited mobility. The syndrome often results from the accumulation of calcium phosphate crystals in the joint, causing inflammation and tissue damage. Early diagnosis and treatment are crucial to manage symptoms and improve quality of life. In this blog post, we'll uncover 28 essential facts about Milwaukee Shoulder Syndrome, helping you understand its causes, symptoms, and treatment options. Whether you're a patient, caregiver, or just curious, these insights will shed light on this debilitating condition.
Key Takeaways:
- Milwaukee Shoulder Syndrome is a rare condition that causes severe shoulder pain and limited mobility, primarily affecting older adults, especially women over 70. Early diagnosis and pain management are crucial for improving quality of life.
- While there is no cure for Milwaukee Shoulder Syndrome, treatments like physical therapy, corticosteroid injections, and surgery can help manage symptoms. Lifestyle changes, regular exercise, and support groups can also make a difference in living with the condition.
What is Milwaukee Shoulder Syndrome?
Milwaukee Shoulder Syndrome (MSS) is a rare and painful condition that affects the shoulder joint. It involves the accumulation of calcium crystals in the joint, leading to severe inflammation and damage. Here are some intriguing facts about this unusual syndrome.
-
Rare Condition: MSS is extremely rare, with only a few hundred cases reported worldwide.
-
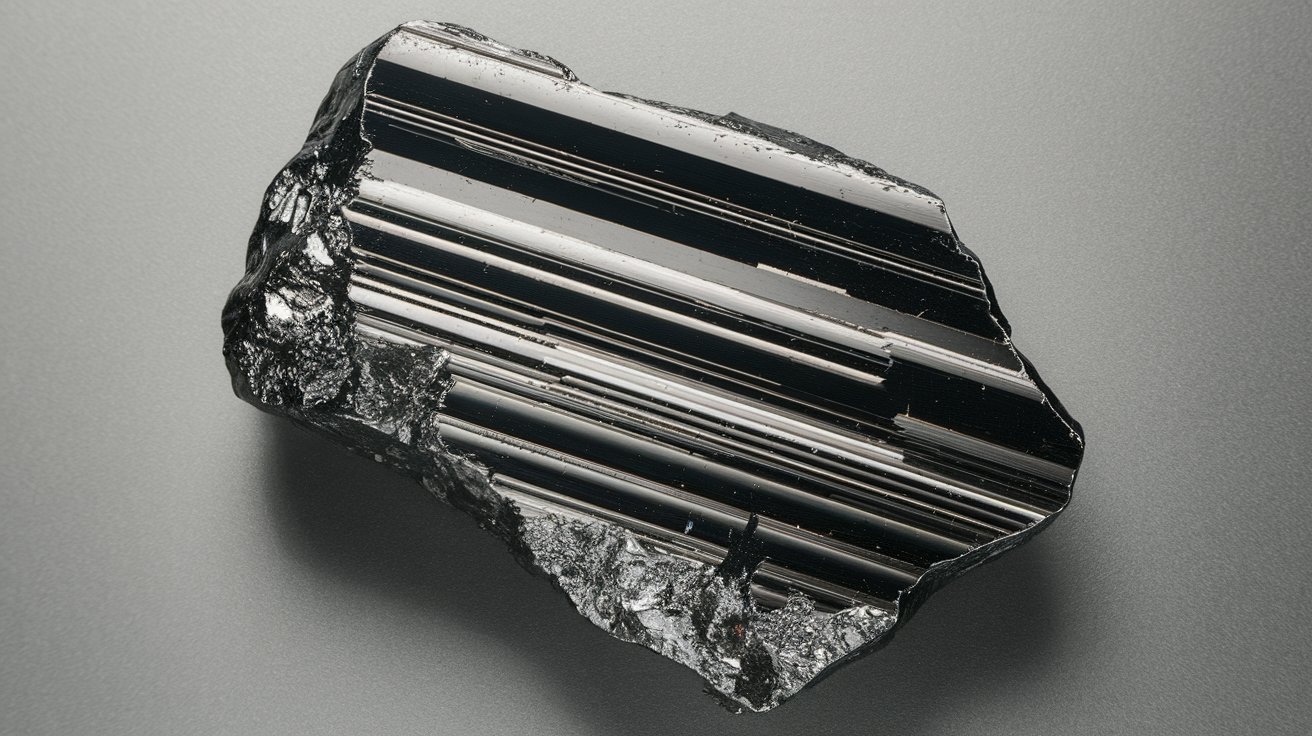
Calcium Crystals: The syndrome is characterized by the deposition of hydroxyapatite and calcium pyrophosphate dihydrate crystals in the shoulder joint.
-
Older Adults: It primarily affects older adults, especially women over the age of 70.
-
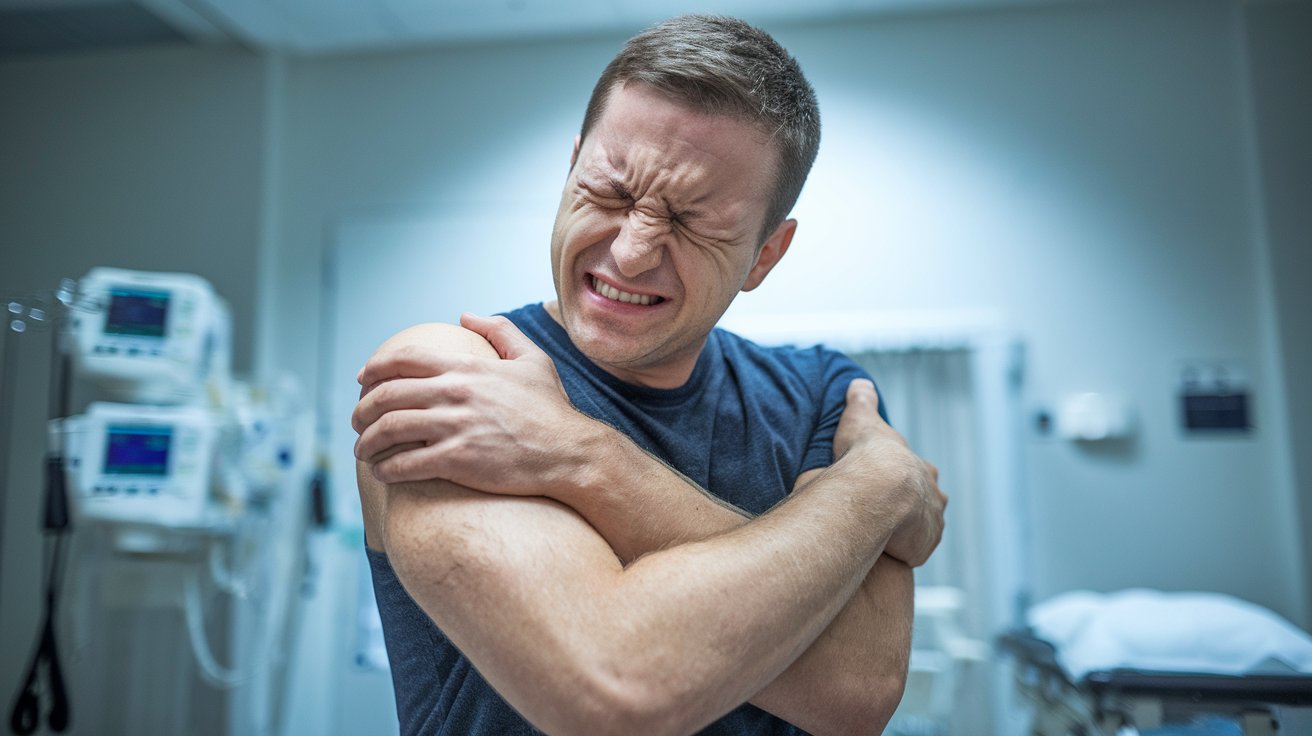
Symptoms: Common symptoms include severe shoulder pain, swelling, and limited range of motion.
-
Joint Destruction: Over time, the accumulation of crystals can lead to significant joint destruction and degeneration.
Causes and Risk Factors
Understanding the causes and risk factors of MSS can help in early detection and management. Here are some key points to consider.
-
Unknown Cause: The exact cause of MSS remains unknown, making it a challenging condition to prevent.
-
Age Factor: Age is a significant risk factor, with most cases occurring in individuals over 70.
-
Gender Predisposition: Women are more likely to develop MSS than men.
-
Previous Joint Injury: A history of shoulder injuries or surgeries can increase the risk of developing MSS.
-
Genetic Factors: There may be a genetic predisposition, although this is not well understood.
Diagnosis and Detection
Early diagnosis is crucial for managing MSS effectively. Here are some facts about how this condition is diagnosed.
-
X-rays: X-rays can reveal the presence of calcium deposits in the shoulder joint.
-
MRI Scans: MRI scans provide detailed images of the joint, helping to assess the extent of damage.
-
Joint Aspiration: Extracting fluid from the joint and analyzing it for crystals can confirm the diagnosis.
-
Blood Tests: Blood tests may be conducted to rule out other conditions with similar symptoms.
-
Physical Examination: A thorough physical examination by a healthcare professional is essential for diagnosis.
Treatment Options
While there is no cure for MSS, several treatment options can help manage symptoms and improve quality of life.
-
Pain Management: Pain relief is a primary focus, often involving medications like NSAIDs.
-
Physical Therapy: Physical therapy can help maintain joint function and reduce stiffness.
-
Corticosteroid Injections: These injections can reduce inflammation and provide temporary relief.
-
Joint Aspiration: Removing excess fluid from the joint can alleviate pain and swelling.
-
Surgery: In severe cases, surgical intervention may be necessary to remove damaged tissue or replace the joint.
Living with Milwaukee Shoulder Syndrome
Living with MSS can be challenging, but understanding the condition and adopting certain lifestyle changes can make a difference.
-
Regular Exercise: Gentle exercises can help maintain joint mobility and strength.
-
Healthy Diet: A balanced diet rich in anti-inflammatory foods can support overall health.
-
Pain Management Techniques: Techniques like heat therapy, cold packs, and relaxation exercises can help manage pain.
-
Support Groups: Joining support groups can provide emotional support and practical advice from others with similar experiences.
-
Regular Check-ups: Regular medical check-ups are essential to monitor the condition and adjust treatment as needed.
Research and Future Directions
Ongoing research aims to better understand MSS and develop more effective treatments. Here are some exciting developments.
-
New Medications: Researchers are exploring new medications that target the underlying causes of MSS.
-
Genetic Studies: Genetic studies may provide insights into the hereditary aspects of the syndrome.
-
Advanced Imaging Techniques: Improved imaging techniques are helping to diagnose MSS earlier and more accurately.
Final Thoughts on Milwaukee Shoulder Syndrome
Milwaukee Shoulder Syndrome, though rare, can severely impact those affected. Understanding its symptoms, causes, and treatment options is crucial for early diagnosis and effective management. This condition primarily affects older women and involves the accumulation of calcium crystals in the shoulder joint, leading to pain, swelling, and limited mobility. Early intervention with anti-inflammatory medications, physical therapy, and sometimes surgery can significantly improve quality of life. Staying informed about this condition helps in recognizing early signs and seeking timely medical advice. While it may not be a common topic, awareness can make a big difference for those who encounter it. Remember, knowledge is power when dealing with any health issue. Stay proactive, consult healthcare professionals, and don't ignore persistent shoulder pain.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.