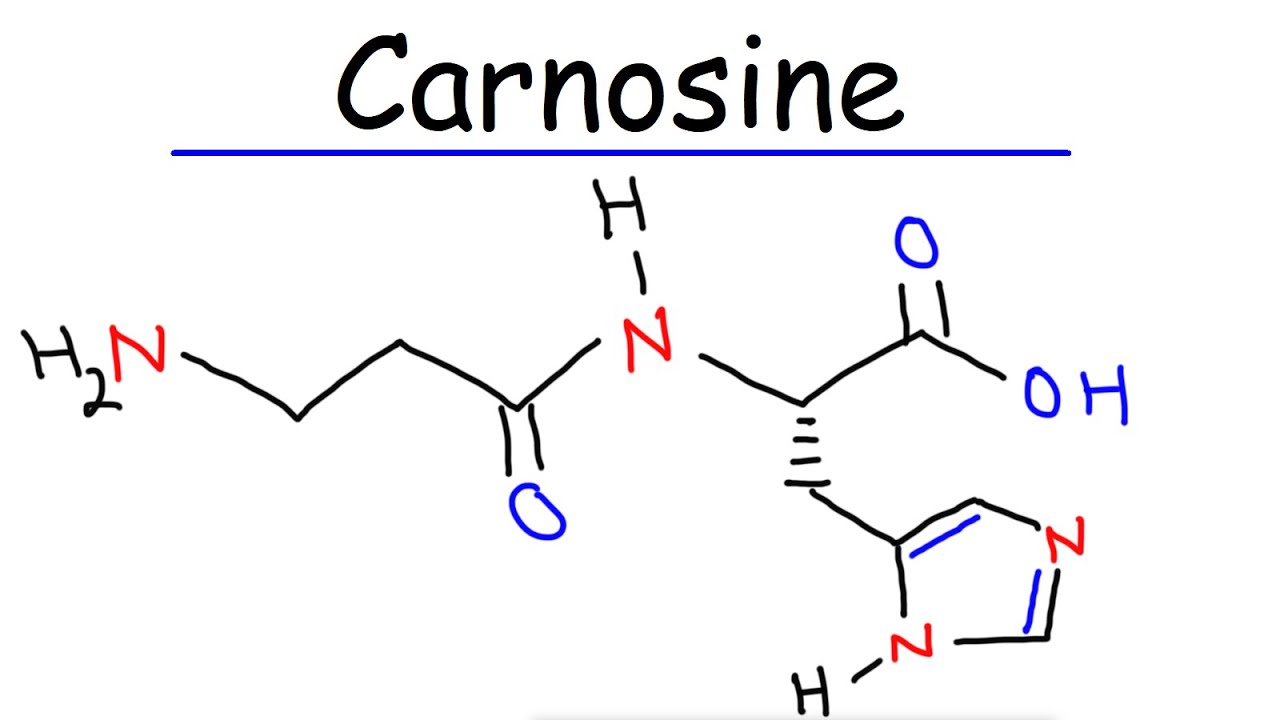
Carnosinemia is a rare metabolic disorder that affects the body's ability to break down carnosine, a dipeptide composed of beta-alanine and L-histidine. This condition is caused by a deficiency in the enzyme carnosinase, leading to the accumulation of carnosine in the blood and urine. Carnosinemia is inherited in an autosomal recessive pattern, meaning a child must inherit one defective gene from each parent to develop the disorder. Symptoms can vary widely, ranging from developmental delays and intellectual disabilities to seizures and muscle weakness. Diagnosing carnosinemia involves clinical evaluation, laboratory tests, and genetic analysis. While there is no specific treatment, managing symptoms and supporting affected individuals is crucial.
Key Takeaways:
- Carnosinemia is a rare disorder caused by a genetic deficiency of carnosinase, leading to developmental delays, seizures, and muscle weakness. Diagnosis involves genetic testing and management focuses on symptom alleviation.
- Research into carnosinemia and carnosinase activity could lead to new diagnostic markers and treatment options for neurological disorders. Understanding the biochemical aspects is crucial for future therapeutic applications.
What is Carnosinemia?
Carnosinemia is a rare metabolic disorder that affects the body's ability to break down carnosine, a dipeptide composed of beta-alanine and L-histidine. This condition can lead to various symptoms and complications. Let's explore some key facts about carnosinemia.
-
Definition and Prevalence
Carnosinemia is caused by a deficiency of carnosinase, an enzyme that splits dipeptides into amino acids. It is quite rare, with an estimated prevalence at birth ranging from 1 in 100,000 to 1 in 1 million worldwide. -
Causes
The primary cause is a genetic deficiency of carnosinase. This autosomal recessive disorder requires a child to inherit one defective gene from each parent. The genetic locus associated with carnosinemia is linked to the carnosinase gene (CNSN).
Symptoms of Carnosinemia
Symptoms can vary widely among individuals with carnosinemia. Some may be asymptomatic, while others experience severe developmental and neurological issues.
-
Developmental Delays
Children with carnosinemia often face significant developmental delays, including slow growth, low muscle tone, and motor delays. By age 2, many show varying degrees of intellectual disabilities. -
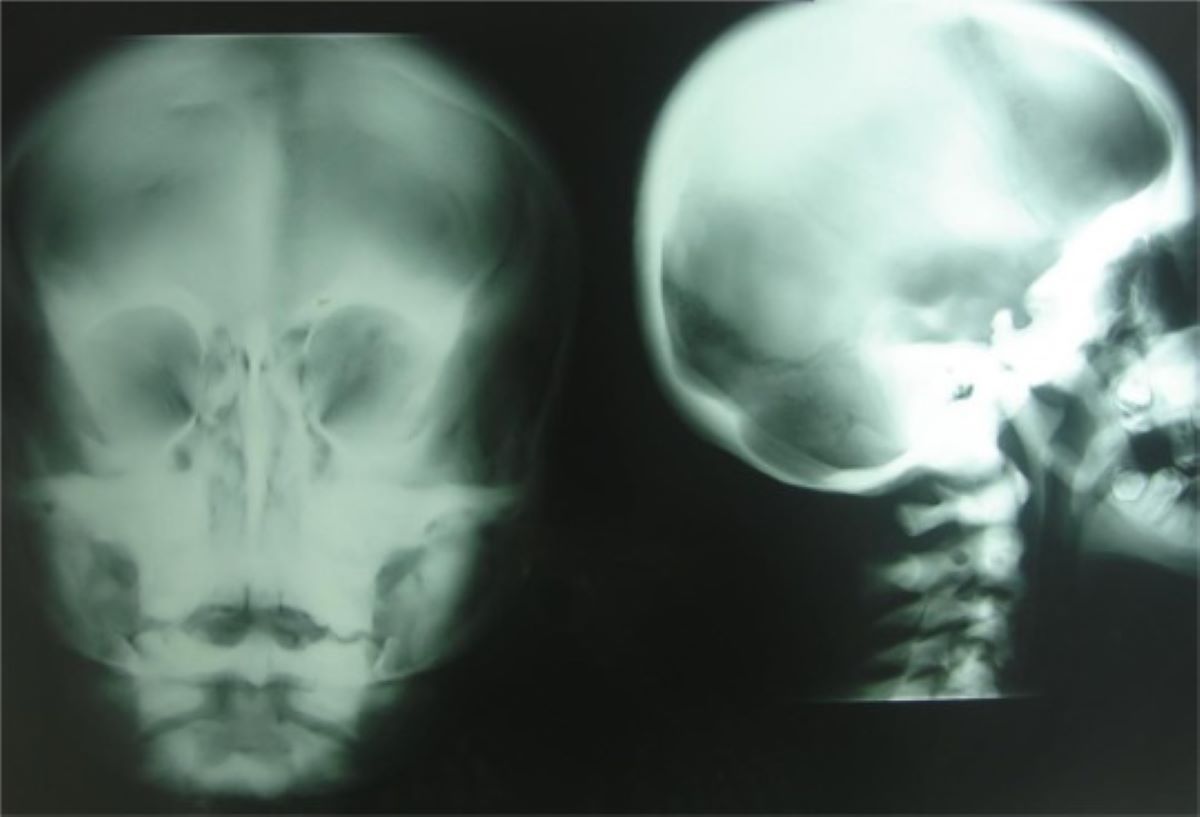
Seizures
Seizures are common in carnosinemia patients. These can include myoclonic seizures, characterized by involuntary jerking movements. EEG tests often reveal abnormal brain activity in these individuals. -
Intellectual Disability
Intellectual disability is a significant consequence. The degree of cognitive impairment varies, but many affected individuals struggle with learning, communication, and daily tasks. -
Muscle Weakness
Some patients experience congenital myopathy, leading to muscle weakness from birth. This can result in poor motor function and mobility issues.
Genetic Basis and Diagnosis
Understanding the genetic basis and diagnostic methods for carnosinemia is crucial for managing the condition.
-
Genetic Basis
Carnosinemia is inherited in an autosomal recessive pattern. A child must inherit one defective gene from each parent to develop the condition. The carnosinase gene (CNSN) is the genetic locus associated with carnosinemia. -
Diagnosis
Diagnosing carnosinemia involves clinical evaluation, laboratory tests, and genetic analysis. Blood tests measure serum carnosinase activity, which is typically low in affected individuals. Urine tests may reveal elevated levels of carnosine and anserine. -
Genetic Testing
Genetic testing can confirm carnosinemia by identifying mutations in the carnosinase gene (CNSN). This is particularly useful for families with a history of the disorder, helping to identify carriers and affected individuals.
Treatment and Management
While there is no specific cure for carnosinemia, various management strategies can help alleviate symptoms and support affected individuals.
-
Treatment
Management focuses on alleviating symptoms. This may include anticonvulsant medications to control seizures, physical therapy to improve motor function, and educational support for intellectual disabilities. -
Dietary Considerations
Although there are no specific dietary restrictions, monitoring the intake of carnosine and anserine is essential. These dipeptides accumulate in the urine due to enzyme deficiency and serve as diagnostic markers.
Biochemical Aspects
Understanding the biochemical aspects of carnosinemia can provide insights into its effects and potential therapeutic approaches.
-
Carnosine and Anserine
Carnosine and anserine are dipeptides composed of beta-alanine and either L-histidine or 1-methylhistidine. In carnosinemia, the hydrolysis of these dipeptides is impaired, leading to their accumulation in the urine. -
Carnosinase Enzyme
Carnosinase (EC 3.4.3.3) breaks down carnosine and anserine into their constituent amino acids. A deficiency in this enzyme leads to the accumulation of these dipeptides and associated symptoms. -
Carnosine's Biological Effects
Carnosine has several beneficial effects, including antioxidant properties. It scavenges reactive oxygen species (ROS) and opposes glycation. Carnosine also chelates divalent metal ions, contributing to its neuroprotective effects.
Carnosinase Deficiency and Neurological Disorders
Carnosinase deficiency has been linked to various neurological disorders, highlighting the importance of understanding this enzyme's role.
-
Carnosinase Deficiency and Neurological Disorders
Reduced carnosinase activity has been associated with progressive mental deficiency, developmental delay, spastic paraplegia, seizures, neurosensory hearing loss, retinitis pigmentosa, and progressive dementia. -
Carnosinase Activity in Aging
Carnosinase activity increases with aging, suggesting a role in age-related diseases. Some neurological disorders, like mild dementia, are characterized by reduced carnosinase levels, highlighting a complex relationship between carnosinase activity and neurological health.
Potential Biomarkers and Future Research
Research into carnosinemia and carnosinase activity could lead to new diagnostic markers and treatment options.
-
Potential Biomarkers
Serum carnosinase levels have been proposed as a potential biomarker for Alzheimer's disease (AD). The presence of carnosinase in cerebrospinal fluid (CSF) could provide insights into AD pathology and serve as a diagnostic tool. -
Future Research Directions
Understanding the carnosinase-carnosine system is crucial for developing strategies to prevent or cure brain-related diseases. Future research should focus on the biochemical mechanisms underlying carnosinemia and potential therapeutic applications of carnosine and its derivatives. -
Carnosine Supplementation
Carnosine supplementation is used among athletes to increase muscle carnosine levels, improving exercise performance and reducing muscle fatigue. However, its use in clinical settings, particularly for carnosinemia patients, is limited due to the enzyme deficiency. -
Carnosinase Deficiency and Neurological Disorders
Reduced carnosinase activity may contribute to various neurological conditions by impairing the normal metabolism of carnosine and related dipeptides. Understanding this relationship could lead to novel diagnostic markers and treatment options.
Key Takeaways on Carnosinemia
Carnosinemia is a rare metabolic disorder caused by a deficiency of the enzyme carnosinase. This condition leads to the accumulation of carnosine and anserine in the body, resulting in various symptoms like developmental delays, seizures, intellectual disability, and muscle weakness. Diagnosing carnosinemia involves clinical evaluation, laboratory tests, and genetic analysis. While there’s no specific treatment, managing symptoms through medications, physical therapy, and educational support can improve the quality of life for affected individuals. Understanding the genetic basis and biochemical mechanisms of carnosinemia is crucial for developing potential therapies. Ongoing research into carnosine and its derivatives holds promise for better management of this condition. By raising awareness and supporting further studies, we can hope for improved outcomes for those living with carnosinemia.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.