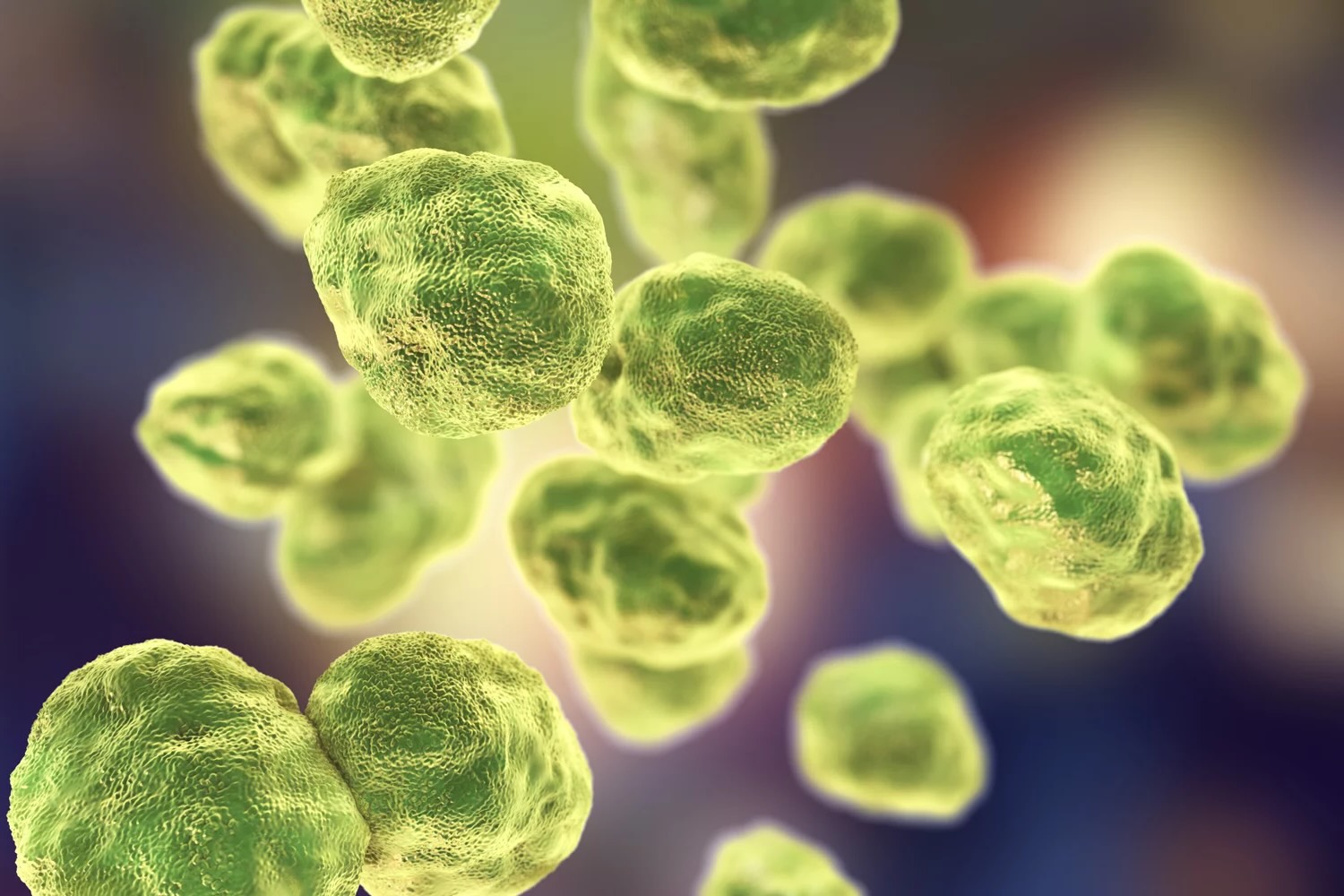
Tularemia, also known as rabbit fever, is a rare but serious infectious disease caused by the bacterium Francisella tularensis. This illness can affect both animals and humans, often spreading through insect bites, direct contact with infected animals, or contaminated food and water. Symptoms can vary widely, ranging from fever and skin ulcers to more severe respiratory issues. Understanding tularemia is crucial for preventing its spread and ensuring proper treatment. In this blog post, we'll explore 50 fascinating facts about tularemia, shedding light on its history, transmission, symptoms, and treatment options. Get ready to dive into the world of this intriguing disease and learn how to stay safe!
Key Takeaways:
- Tularemia, also known as rabbit fever, is a rare infectious disease caused by the bacterium Francisella tularensis. It can be transmitted through insect bites, contact with infected animals, contaminated food or water, and inhalation of aerosols.
- Recognizing the symptoms of tularemia is crucial for timely treatment. The disease can present in several forms, such as skin ulcers, swollen lymph nodes, eye inflammation, throat pain, and severe respiratory symptoms. Early treatment with antibiotics is essential for recovery.
What is Tularemia?
Tularemia, also known as rabbit fever, is a rare infectious disease caused by the bacterium Francisella tularensis. It primarily affects animals, especially rodents, rabbits, and hares, but can also infect humans. Here are some intriguing facts about this disease.
- Tularemia is named after Tulare County, California, where the disease was first identified in ground squirrels.
- The bacterium Francisella tularensis is highly infectious, with as few as 10 organisms needed to cause disease.
- There are two main subspecies of Francisella tularensis: tularensis (Type A) and holarctica (Type B). Type A is more virulent.
- Tularemia can be transmitted through various routes, including insect bites, direct contact with infected animals, ingestion of contaminated water or food, and inhalation of aerosols.
- The disease is considered a potential bioterrorism agent due to its high infectivity and ability to be aerosolized.
Symptoms and Diagnosis
Recognizing the symptoms of tularemia is crucial for timely treatment. The disease can present in several forms, depending on the route of infection.
- Ulceroglandular tularemia is the most common form, characterized by skin ulcers and swollen lymph glands.
- Glandular tularemia presents with swollen lymph nodes but no skin ulcers.
- Oculoglandular tularemia occurs when the bacteria enter through the eye, causing eye inflammation and swollen lymph nodes.
- Oropharyngeal tularemia results from ingesting contaminated food or water, leading to throat pain, mouth ulcers, and swollen lymph nodes.
- Pneumonic tularemia is the most severe form, caused by inhaling the bacteria, leading to cough, chest pain, and difficulty breathing.
- Typhoidal tularemia is a rare form that causes fever, exhaustion, and weight loss without localized symptoms.
- Diagnosis is typically confirmed through blood tests, cultures, or PCR (polymerase chain reaction) testing.
Treatment and Prevention
Effective treatment and preventive measures can significantly reduce the impact of tularemia.
- Antibiotics such as streptomycin, gentamicin, doxycycline, and ciprofloxacin are effective against tularemia.
- Early treatment is crucial to prevent complications and reduce the risk of severe illness.
- There is no widely available vaccine for tularemia, but research is ongoing.
- Preventive measures include using insect repellent, wearing protective clothing, and avoiding contact with wild animals.
- Cooking meat thoroughly and drinking only treated water can help prevent infection.
Historical and Geographical Context
Understanding the history and distribution of tularemia provides insight into its impact on human and animal populations.
- Tularemia was first described in 1911 by Dr. Edward Francis, who identified the bacterium in ground squirrels.
- The disease has been reported in North America, Europe, Asia, and parts of Africa.
- In the United States, tularemia is most commonly found in the central and southern states.
- Sweden and Finland have the highest incidence rates of tularemia in Europe.
- Outbreaks have occurred in various countries, often linked to specific environmental conditions or activities.
Wildlife and Environmental Factors
The role of wildlife and environmental factors in the spread of tularemia is significant.
- Rodents, rabbits, and hares are the primary reservoirs of Francisella tularensis.
- Ticks, deer flies, and mosquitoes can transmit the bacteria to humans and animals.
- Tularemia outbreaks often occur in rural areas where people are more likely to come into contact with infected animals or insects.
- Environmental changes, such as flooding or land development, can influence the spread of tularemia by altering animal habitats.
- Hunters, trappers, and outdoor enthusiasts are at higher risk of contracting tularemia due to increased exposure to wildlife.
Public Health and Awareness
Raising awareness about tularemia is essential for public health and safety.
- Public health campaigns can educate people about the risks and preventive measures for tularemia.
- Healthcare providers should be aware of the symptoms and diagnostic methods for tularemia, especially in endemic areas.
- Reporting and monitoring tularemia cases can help track outbreaks and implement control measures.
- Collaboration between wildlife biologists, veterinarians, and public health officials is crucial for managing tularemia.
- Research on tularemia can lead to better diagnostic tools, treatments, and potential vaccines.
Interesting Facts and Trivia
Some lesser-known facts about tularemia add to the intrigue of this disease.
- Tularemia can survive in water, soil, and animal carcasses for weeks to months.
- The bacterium is highly resistant to environmental stress, making it a formidable pathogen.
- Tularemia has been used in biological warfare research due to its high infectivity and potential for aerosol transmission.
- The disease can affect a wide range of animals, including birds, reptiles, and fish.
- Tularemia is sometimes called "rabbit fever" because it is often associated with rabbits and hares.
- The bacterium Francisella tularensis is named after Dr. Edward Francis, who made significant contributions to understanding the disease.
- Tularemia can cause significant economic losses in the fur industry due to its impact on wild animal populations.
- The disease has been reported in domestic animals, including cats, dogs, and livestock.
- Tularemia can be transmitted through bites or scratches from infected animals, including pets.
- The incubation period for tularemia ranges from 1 to 14 days, with most cases occurring within 3 to 5 days of exposure.
- Tularemia is not known to be transmitted from person to person, reducing the risk of widespread outbreaks.
- The disease can cause long-term health effects, including chronic fatigue and joint pain, if not treated promptly.
- Tularemia is considered a zoonotic disease, meaning it can be transmitted from animals to humans.
- The bacterium Francisella tularensis is classified as a Category A bioterrorism agent by the Centers for Disease Control and Prevention (CDC).
- Tularemia can be challenging to diagnose due to its varied symptoms and similarity to other illnesses.
- The disease has been studied extensively in laboratory settings to understand its pathogenesis and develop effective treatments.
- Tularemia outbreaks have been linked to activities such as farming, landscaping, and construction, which can disturb contaminated soil or water.
- Public awareness and education about tularemia can help reduce the risk of infection and promote early diagnosis and treatment.
Tularemia: Key Points to Remember
Tularemia, also known as rabbit fever, is a rare but serious disease caused by the bacterium Francisella tularensis. It primarily affects small mammals like rabbits and rodents but can also infect humans. Transmission occurs through insect bites, direct contact with infected animals, or inhalation of contaminated particles. Symptoms vary depending on the route of infection, ranging from skin ulcers to severe respiratory issues.
Early diagnosis and treatment with antibiotics are crucial for recovery. Preventive measures include using insect repellent, wearing protective clothing, and avoiding handling wild animals. Public awareness and education about tularemia can help reduce the risk of infection.
Understanding these key points can help you stay informed and safe. Tularemia may be rare, but knowing the facts can make a big difference in preventing and managing this disease.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
