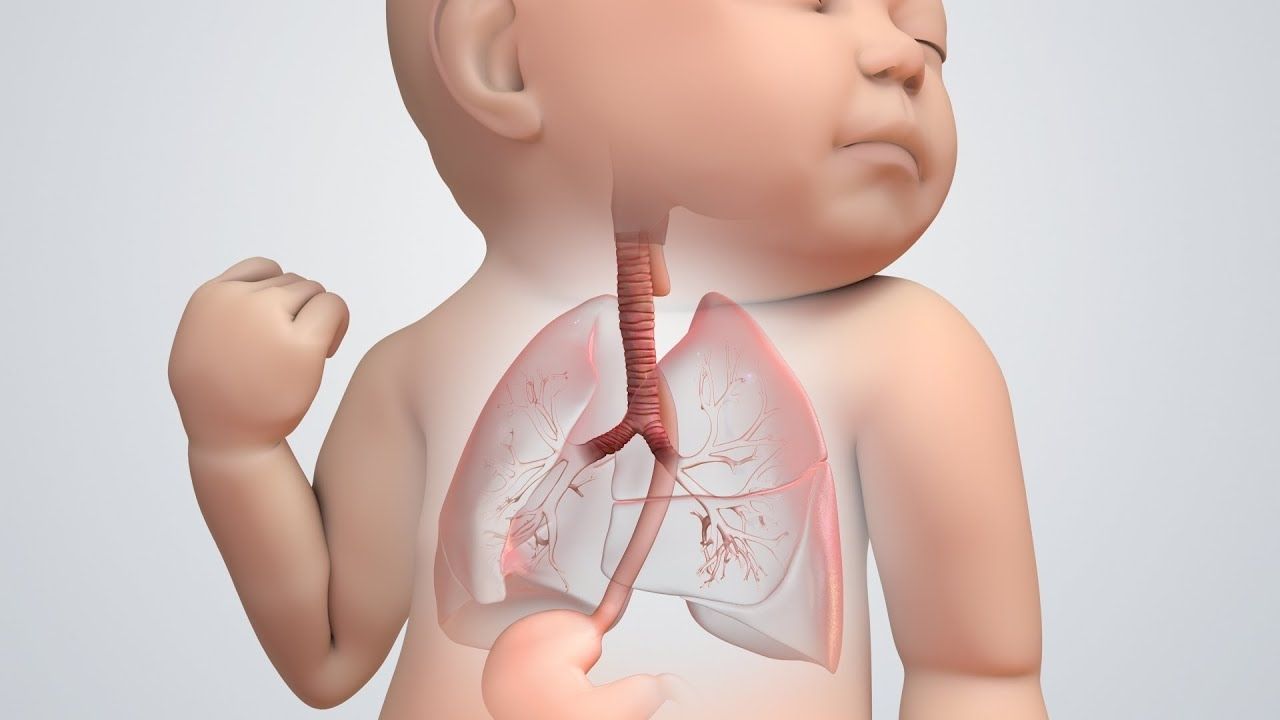
What is a tracheoesophageal fistula? A tracheoesophageal fistula (TEF) is a rare birth defect where an abnormal connection forms between the trachea (windpipe) and the esophagus (food pipe). This condition can cause serious problems with breathing and swallowing. Babies with TEF often have difficulty feeding, leading to choking or coughing when they try to eat. TEF usually requires surgical intervention soon after birth to correct the connection and allow the baby to eat and breathe normally. Understanding the symptoms and treatment options is crucial for parents and caregivers. Let's dive into 50 facts about this condition to provide a comprehensive overview.
Key Takeaways:
- Tracheoesophageal fistula (TEF) is a rare condition where the trachea and esophagus connect abnormally, causing breathing and feeding difficulties in newborns. Early diagnosis and surgical intervention are crucial for survival.
- Children with TEF can lead healthy lives with proper treatment and support. Regular monitoring and access to resources, such as support groups and genetic counseling, are essential for managing the condition.
What is Tracheoesophageal Fistula?
Tracheoesophageal fistula (TEF) is a rare congenital condition where an abnormal connection forms between the trachea and esophagus. This condition can cause severe complications in newborns, affecting their ability to breathe and eat properly. Here are some intriguing facts about TEF.
- TEF occurs in approximately 1 in 3,500 live births.
- It is often associated with esophageal atresia, where the esophagus does not form correctly.
- The exact cause of TEF remains unknown, though genetic and environmental factors may play a role.
- TEF can be diagnosed prenatally through ultrasound or MRI.
- Symptoms in newborns include coughing, choking, and difficulty breathing during feeding.
- TEF is more common in males than females.
- There are five types of TEF, with Type C being the most common.
- TEF can be part of a syndrome called VACTERL, which includes vertebral, anal, cardiac, tracheal, esophageal, renal, and limb anomalies.
- Early surgical intervention is crucial for the survival of infants with TEF.
- Post-surgery, babies may require a feeding tube until they can eat normally.
Diagnosis and Symptoms
Understanding the diagnosis and symptoms of TEF is essential for early intervention. Here are some key points to consider.
- TEF is often suspected if a newborn has excessive drooling or difficulty swallowing.
- A chest X-ray can help confirm the diagnosis by showing air in the stomach.
- Contrast studies, where a dye is swallowed, can outline the esophagus and trachea.
- Bronchoscopy and endoscopy are used to visualize the fistula directly.
- TEF can sometimes be detected during routine prenatal screenings.
- Infants with TEF may have recurrent respiratory infections.
- Cyanosis, or a bluish tint to the skin, can occur due to breathing difficulties.
- TEF can lead to aspiration pneumonia if food or liquid enters the lungs.
- Some babies with TEF may have a distended abdomen due to trapped air.
- Immediate medical attention is required if TEF is suspected in a newborn.
Treatment and Management
Treating TEF involves a combination of surgical and supportive care. Here are some important aspects of treatment and management.
- The primary treatment for TEF is surgical repair to close the fistula.
- Surgery is usually performed within the first few days of life.
- In some cases, multiple surgeries may be needed to fully correct the condition.
- Postoperative care includes monitoring for complications like leaks or strictures.
- Babies may need mechanical ventilation to assist with breathing after surgery.
- Gastrostomy tubes are often placed to provide nutrition until oral feeding is safe.
- Long-term follow-up is necessary to monitor growth and development.
- Speech therapy may be required if vocal cord damage occurs during surgery.
- Some children may experience gastroesophageal reflux disease (GERD) after TEF repair.
- Regular check-ups with a pediatric surgeon and gastroenterologist are essential.
Long-term Outcomes and Complications
Living with TEF can present challenges, but many children go on to lead healthy lives. Here are some facts about long-term outcomes and potential complications.
- Most children with TEF achieve normal growth and development.
- Some may have persistent feeding difficulties and require ongoing therapy.
- Respiratory issues, such as chronic cough or wheezing, can occur in some children.
- Strictures, or narrowing of the esophagus, may develop and require dilation.
- TEF repair can sometimes lead to tracheomalacia, where the trachea is weak and collapses.
- Regular monitoring for esophageal motility disorders is important.
- Psychological support may be beneficial for children and families coping with TEF.
- Participation in support groups can provide valuable resources and community.
- Advances in surgical techniques have improved the prognosis for TEF patients.
- Research is ongoing to better understand the causes and improve treatments for TEF.
Support and Resources
Support and resources are crucial for families dealing with TEF. Here are some helpful points to consider.
- Many hospitals have specialized teams for managing congenital anomalies like TEF.
- Genetic counseling can provide information on the risk of recurrence in future pregnancies.
- Early intervention programs can help with developmental delays.
- Online communities and forums offer support and advice from other families.
- Nonprofit organizations provide resources and advocacy for TEF awareness.
- Educational materials can help parents understand the condition and care requirements.
- Financial assistance programs may be available for medical expenses.
- Social workers can assist with navigating healthcare systems and accessing services.
- Pediatricians play a key role in coordinating care and monitoring progress.
- Emotional support from family and friends is invaluable for coping with TEF.
Final Thoughts on Tracheoesophageal Fistula
Tracheoesophageal fistula (TEF) is a serious condition that affects newborns, causing abnormal connections between the trachea and esophagus. Early diagnosis and treatment are crucial for improving outcomes. Symptoms like difficulty breathing, coughing, and feeding problems often signal the need for medical attention. Surgery is the primary treatment, aiming to separate the trachea and esophagus and close the fistula. Post-surgery, most children lead healthy lives, though some may face long-term issues like GERD or respiratory infections. Awareness and understanding of TEF can help parents and caregivers provide better care and support. Always consult healthcare professionals for accurate information and guidance. By staying informed, you can make a significant difference in the lives of those affected by TEF.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
