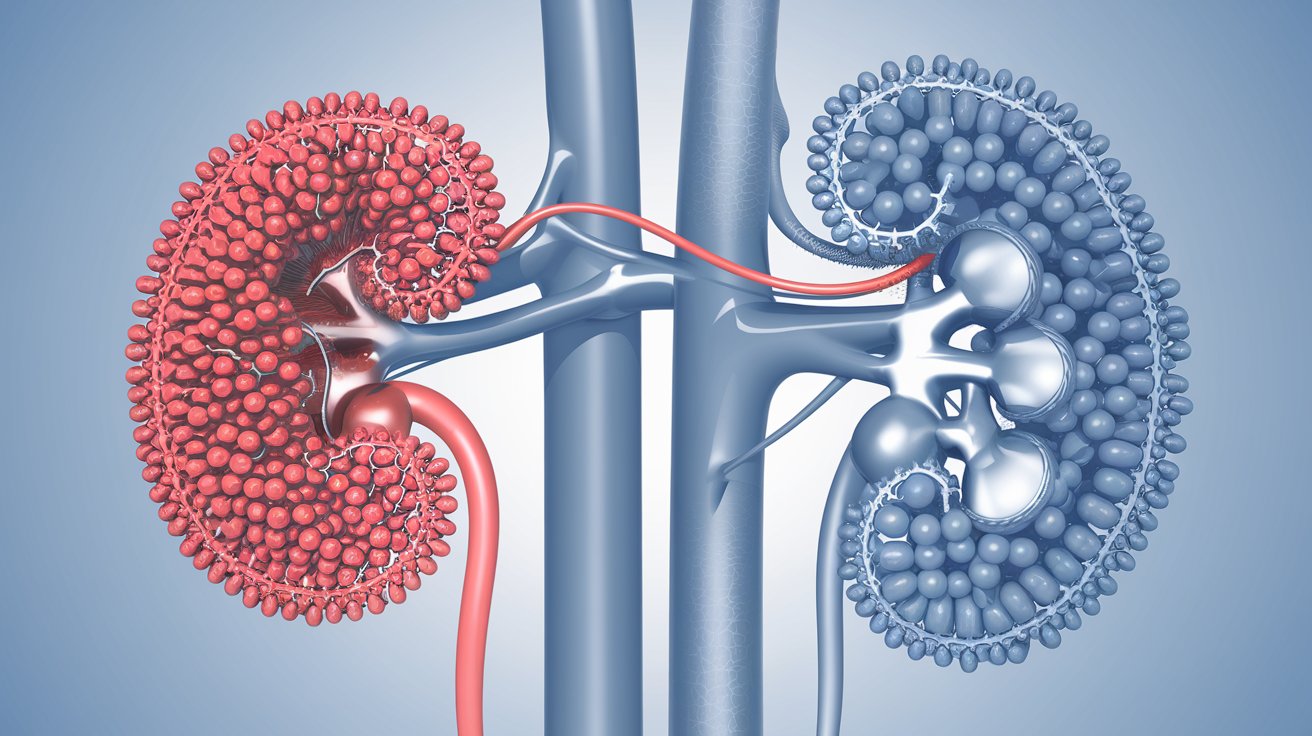
Renal Tubular Acidosis (RTA) is a condition where the kidneys fail to properly acidify urine, leading to a buildup of acid in the blood. This disorder can cause various symptoms, including fatigue, muscle weakness, and growth delays in children. Understanding RTA is crucial for managing its effects and improving quality of life. This article will provide 50 essential facts about Renal Tubular Acidosis, covering its types, causes, symptoms, diagnosis, and treatment options. Whether you're a patient, caregiver, or just curious, these facts will help you grasp the complexities of this condition. Let's dive into the world of RTA and uncover what you need to know.
Key Takeaways:
- Renal Tubular Acidosis (RTA) is a group of kidney disorders that can cause fatigue, muscle weakness, and kidney stones. It's diagnosed through urine and blood tests, and treatment involves medication and lifestyle changes.
- Living with RTA requires regular medical care, a balanced diet, and staying active. Avoiding alcohol and smoking, educating family members, and seeking mental health support are important for managing this condition.
What is Renal Tubular Acidosis?
Renal Tubular Acidosis (RTA) is a medical condition where the kidneys fail to properly acidify urine. This can lead to various health issues due to the imbalance of acid and base in the body. Here are some intriguing facts about RTA.
- RTA is not a single disease but a group of disorders that affect kidney function.
- It can be inherited or acquired due to other medical conditions.
- There are four main types of RTA: Type 1 (Distal), Type 2 (Proximal), Type 3 (Mixed), and Type 4 (Hyperkalemic).
- Type 1 RTA is the most common form and affects the distal tubules of the kidneys.
- Type 2 RTA involves the proximal tubules and is often associated with other conditions like Fanconi syndrome.
- Type 3 RTA is rare and considered a combination of Type 1 and Type 2.
- Type 4 RTA is linked to hyperkalemia, a condition with high potassium levels in the blood.
- Symptoms of RTA can include fatigue, muscle weakness, and growth retardation in children.
- Chronic RTA can lead to kidney stones and bone disease.
- Blood tests measuring bicarbonate levels help diagnose RTA.
Causes and Risk Factors
Understanding what causes RTA and the risk factors involved can help in early detection and management.
- Genetic mutations can cause inherited forms of RTA.
- Autoimmune diseases like Sjögren's syndrome and lupus can lead to acquired RTA.
- Chronic kidney disease is a significant risk factor for developing RTA.
- Certain medications, such as amphotericin B and lithium, can induce RTA.
- Conditions like diabetes and sickle cell anemia increase the risk of RTA.
- RTA can also result from kidney transplant complications.
- Heavy metal poisoning, such as lead or mercury, can cause RTA.
- Dehydration and electrolyte imbalances are common triggers.
- Urinary tract infections can exacerbate RTA symptoms.
- Alcohol abuse is a lesser-known risk factor for RTA.
Diagnosis and Testing
Diagnosing RTA involves a series of tests to confirm the condition and identify its type.
- Urine pH testing is crucial for diagnosing RTA.
- Blood gas analysis helps measure acid-base balance in the body.
- Serum electrolytes, including potassium and bicarbonate, are checked.
- Genetic testing can identify inherited forms of RTA.
- Kidney function tests, like creatinine clearance, assess overall kidney health.
- Imaging studies, such as ultrasounds, can detect kidney stones.
- Bone density scans may be performed to check for bone disease.
- A urine anion gap test helps differentiate between types of RTA.
- Ammonium chloride loading tests can diagnose Type 1 RTA.
- Fractional excretion of bicarbonate is used to diagnose Type 2 RTA.
Treatment and Management
Managing RTA involves addressing the underlying cause and correcting the acid-base imbalance.
- Sodium bicarbonate supplements are commonly used to treat RTA.
- Potassium citrate can help prevent kidney stones in RTA patients.
- Thiazide diuretics are sometimes prescribed for Type 1 RTA.
- Alkali therapy is essential for managing chronic RTA.
- Dietary changes, such as reducing salt intake, can help manage symptoms.
- Regular monitoring of blood and urine tests is crucial for RTA patients.
- Treating underlying conditions, like autoimmune diseases, can improve RTA.
- Avoiding medications that worsen RTA is important.
- Hydration is key to preventing kidney stones in RTA.
- In severe cases, dialysis may be required.
Living with Renal Tubular Acidosis
Living with RTA requires lifestyle adjustments and ongoing medical care.
- Regular follow-ups with a nephrologist are essential.
- Maintaining a balanced diet helps manage acid-base levels.
- Physical activity can improve overall health and well-being.
- Avoiding alcohol and smoking is beneficial.
- Educating family members about RTA can provide support.
- Joining support groups can help cope with the condition.
- Keeping a symptom diary aids in tracking changes and treatment effectiveness.
- Staying informed about new treatments and research is important.
- Mental health support is crucial for coping with chronic illness.
- Early diagnosis and treatment can significantly improve quality of life.
Final Thoughts on Renal Tubular Acidosis
Renal Tubular Acidosis (RTA) isn't just a mouthful; it's a serious condition affecting the kidneys' ability to maintain the body's acid-base balance. Understanding the different types—Type 1, Type 2, and Type 4—helps in recognizing symptoms and seeking timely treatment. Each type has unique causes and treatments, but all require medical attention to prevent complications like kidney stones or bone disease. Staying informed about RTA can make a huge difference in managing the condition effectively. Regular check-ups, a balanced diet, and proper medication can help maintain a good quality of life. If you suspect any symptoms, consult a healthcare provider immediately. Knowledge is power, and being aware of RTA's facts can lead to better health outcomes. Stay proactive, stay healthy!
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
