Phosphoglucomutase Deficiency Type 1 is a rare genetic disorder that affects the body's ability to process glucose properly. This condition can lead to a variety of symptoms, including muscle weakness, exercise intolerance, and episodes of low blood sugar. Understanding this disorder is crucial for those affected and their families, as it can help manage symptoms and improve quality of life. In this blog post, we will explore 50 facts about Phosphoglucomutase Deficiency Type 1, shedding light on its causes, symptoms, diagnosis, and treatment options. Whether you're a patient, caregiver, or simply curious, these facts will provide valuable insights into this complex condition.
Key Takeaways:
- PGM1-CDG is a rare genetic disorder affecting carbohydrate metabolism, causing symptoms like muscle weakness and developmental delays. While there's no cure, treatments like dietary modifications and genetic testing can help manage the condition.
- Living with PGM1-CDG presents unique challenges, but support groups, educational resources, and advocacy organizations are available to help individuals and families. Early diagnosis and intervention can significantly improve outcomes.
What is Phosphoglucomutase Deficiency Type 1?
Phosphoglucomutase Deficiency Type 1 (PGM1-CDG) is a rare genetic disorder affecting carbohydrate metabolism. This condition can lead to various symptoms, impacting multiple body systems. Here are some intriguing facts about PGM1-CDG.
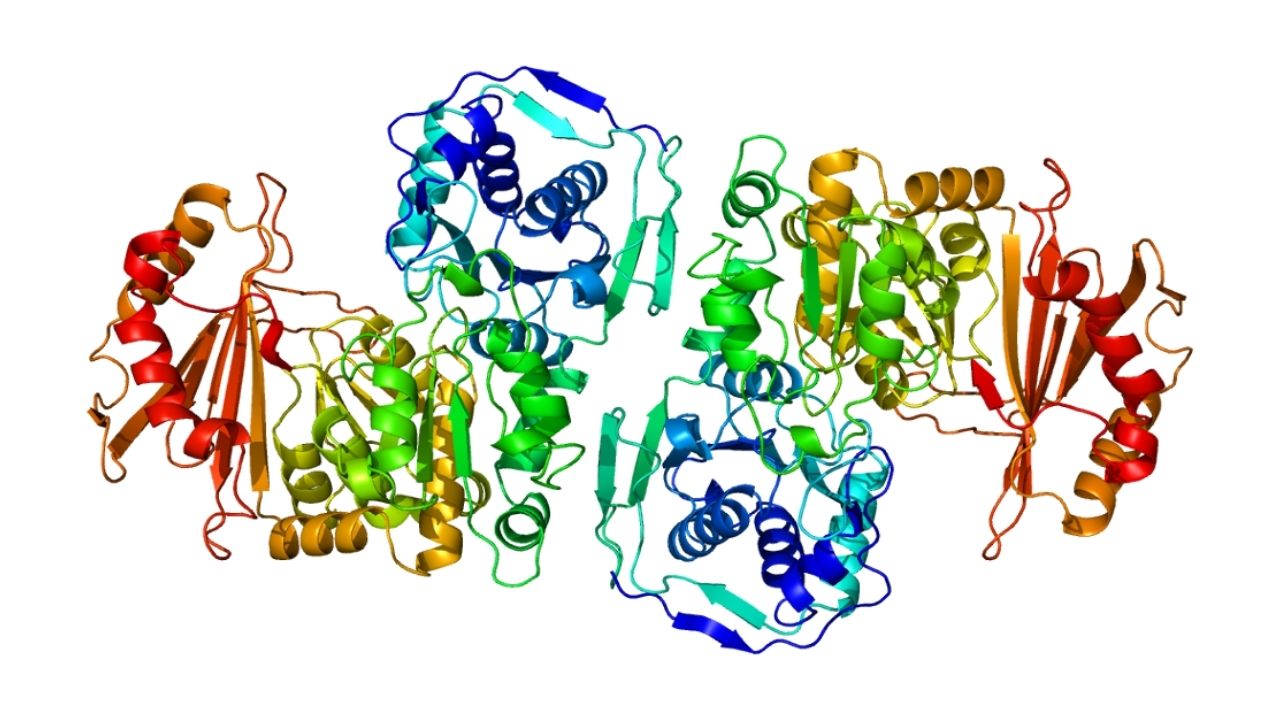
- PGM1-CDG is caused by mutations in the PGM1 gene, which encodes the enzyme phosphoglucomutase 1.
- This enzyme plays a crucial role in converting glucose-1-phosphate to glucose-6-phosphate, a key step in glycogen metabolism.
- PGM1-CDG is classified as a congenital disorder of glycosylation (CDG), a group of inherited metabolic disorders.
- The disorder is inherited in an autosomal recessive manner, meaning both parents must carry a copy of the mutated gene.
- Symptoms can vary widely, even among individuals with the same genetic mutation.
Symptoms and Diagnosis
Understanding the symptoms and how PGM1-CDG is diagnosed can help in early detection and management.
- Common symptoms include muscle weakness, exercise intolerance, and hypoglycemia.
- Some individuals may experience liver dysfunction, leading to elevated liver enzymes.
- Cardiomyopathy, a disease of the heart muscle, can also be a symptom.
- Developmental delays and intellectual disabilities are observed in some patients.
- Blood tests revealing abnormal glycosylation patterns can aid in diagnosis.
- Genetic testing confirms the presence of mutations in the PGM1 gene.
- Newborn screening programs do not typically include PGM1-CDG, making early diagnosis challenging.
Treatment and Management
While there is no cure for PGM1-CDG, various treatments can help manage symptoms and improve quality of life.
- Dietary modifications, such as a high-protein diet, can help manage hypoglycemia.
- Regular monitoring of blood glucose levels is essential for individuals with PGM1-CDG.
- Physical therapy can improve muscle strength and coordination.
- Cardiac care is crucial for those with cardiomyopathy.
- Liver function should be monitored regularly to detect any abnormalities early.
- Some patients may benefit from supplements like D-ribose, which can improve energy levels.
- Multidisciplinary care teams, including geneticists, neurologists, and dietitians, provide comprehensive management.
Genetic and Research Insights
Research into PGM1-CDG continues to uncover new insights and potential treatments.
- The PGM1 gene is located on chromosome 1.
- Over 30 different mutations in the PGM1 gene have been identified in individuals with PGM1-CDG.
- Animal models, such as mice, are used to study the disease and test potential treatments.
- Researchers are exploring gene therapy as a potential future treatment for PGM1-CDG.
- Clinical trials are ongoing to evaluate the effectiveness of various therapeutic approaches.
- Patient registries help researchers collect data and improve understanding of the disease.
- Collaboration between researchers, clinicians, and patient advocacy groups is essential for advancing knowledge and treatment options.
Living with PGM1-CDG
Living with PGM1-CDG presents unique challenges, but support and resources are available to help individuals and families.
- Support groups and online communities provide valuable connections and information.
- Educational resources can help families understand the disease and its management.
- Advocacy organizations work to raise awareness and funding for research.
- Genetic counseling is recommended for families affected by PGM1-CDG.
- Schools and workplaces may need to make accommodations for individuals with PGM1-CDG.
- Mental health support is important for both patients and their families.
- Regular follow-up with healthcare providers ensures optimal management of the condition.
- Emergency plans should be in place for managing hypoglycemic episodes.
Interesting Facts and Statistics
Here are some additional interesting facts and statistics about PGM1-CDG.
- PGM1-CDG is estimated to affect fewer than 1 in 1,000,000 people worldwide.
- The disorder was first described in the medical literature in 2014.
- PGM1-CDG is more commonly diagnosed in individuals of European descent.
- The average age of diagnosis is around 5 years old.
- Early diagnosis and intervention can significantly improve outcomes.
- Some individuals with PGM1-CDG may have mild symptoms and lead relatively normal lives.
- The life expectancy of individuals with PGM1-CDG varies depending on the severity of symptoms and complications.
- Research into PGM1-CDG is funded by various organizations, including the National Institutes of Health (NIH).
- Awareness campaigns aim to educate healthcare providers and the public about PGM1-CDG.
- Advances in genetic testing have improved the ability to diagnose PGM1-CDG accurately.
- Some individuals with PGM1-CDG may develop secondary conditions, such as diabetes or thyroid disorders.
- The disorder can affect both males and females equally.
- PGM1-CDG is one of over 130 known congenital disorders of glycosylation.
- The prevalence of PGM1-CDG may be underestimated due to misdiagnosis or lack of awareness.
- Ongoing research aims to identify additional genetic mutations associated with PGM1-CDG.
- Patient stories and experiences play a crucial role in raising awareness and driving research efforts.
Final Thoughts on Phosphoglucomutase Deficiency Type 1
Phosphoglucomutase Deficiency Type 1 (PGM1) is a rare metabolic disorder that affects how the body processes glucose. Understanding this condition is crucial for those diagnosed and their families. Symptoms can vary widely, from muscle weakness to liver dysfunction, making early diagnosis and treatment essential. Genetic testing plays a significant role in identifying PGM1, and ongoing research aims to improve treatment options.
Living with PGM1 requires a multidisciplinary approach, including dietary management and regular medical check-ups. Support groups and resources can provide emotional and practical help. Awareness and education about PGM1 are vital for better management and quality of life.
By staying informed and proactive, individuals with PGM1 can lead healthier lives. Always consult healthcare professionals for personalized advice and treatment plans. Knowledge is power when dealing with rare conditions like PGM1.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
