Paracoccidioidomycosis is a fungal infection caused by the Paracoccidioides species. Found mainly in Latin America, this disease primarily affects the lungs but can spread to other parts of the body. Symptoms often include cough, fever, weight loss, and skin lesions. Farmers and rural workers are at higher risk due to their exposure to soil. Diagnosis involves identifying the fungus in tissue samples or body fluids. Treatment typically includes antifungal medications like itraconazole or amphotericin B. Early detection and proper medical care are crucial for managing this disease effectively. Understanding paracoccidioidomycosis can help in preventing and treating this serious infection.
Key Takeaways:
- Paracoccidioidomycosis, a fungal infection common in Latin America, primarily affects rural workers and can take years to show symptoms. Early diagnosis and treatment are crucial for better outcomes.
- Preventing Paracoccidioidomycosis involves avoiding soil exposure and wearing protective masks. Ongoing research offers hope for improved treatments and better understanding of this complex disease.
What is Paracoccidioidomycosis?
Paracoccidioidomycosis (PCM) is a fungal infection caused by the Paracoccidioides species. It primarily affects the lungs but can spread to other parts of the body. Here are some intriguing facts about this disease.
-
Paracoccidioidomycosis is endemic in Latin America. Countries like Brazil, Argentina, Colombia, and Venezuela report the highest cases.
-
The disease is caused by inhaling fungal spores. These spores are found in soil and can become airborne, leading to infection when inhaled.
-
It primarily affects rural workers. Farmers and agricultural workers are at higher risk due to their frequent contact with soil.
-
Men are more likely to get PCM. The disease is more common in males, possibly due to hormonal differences that affect immune response.
-
Symptoms can take years to appear. The incubation period can be long, sometimes taking decades for symptoms to manifest.
Symptoms and Diagnosis
Understanding the symptoms and how PCM is diagnosed can help in early detection and treatment.
-
Initial symptoms resemble tuberculosis. Cough, fever, and weight loss are common early signs.
-
Skin lesions are a hallmark of PCM. These lesions often appear on the face and can be mistaken for other skin conditions.
-
PCM can affect the mucous membranes. Ulcers can form in the mouth, nose, and throat, causing pain and difficulty swallowing.
-
Chest X-rays can reveal lung involvement. These images often show nodules or cavities in the lungs.
-
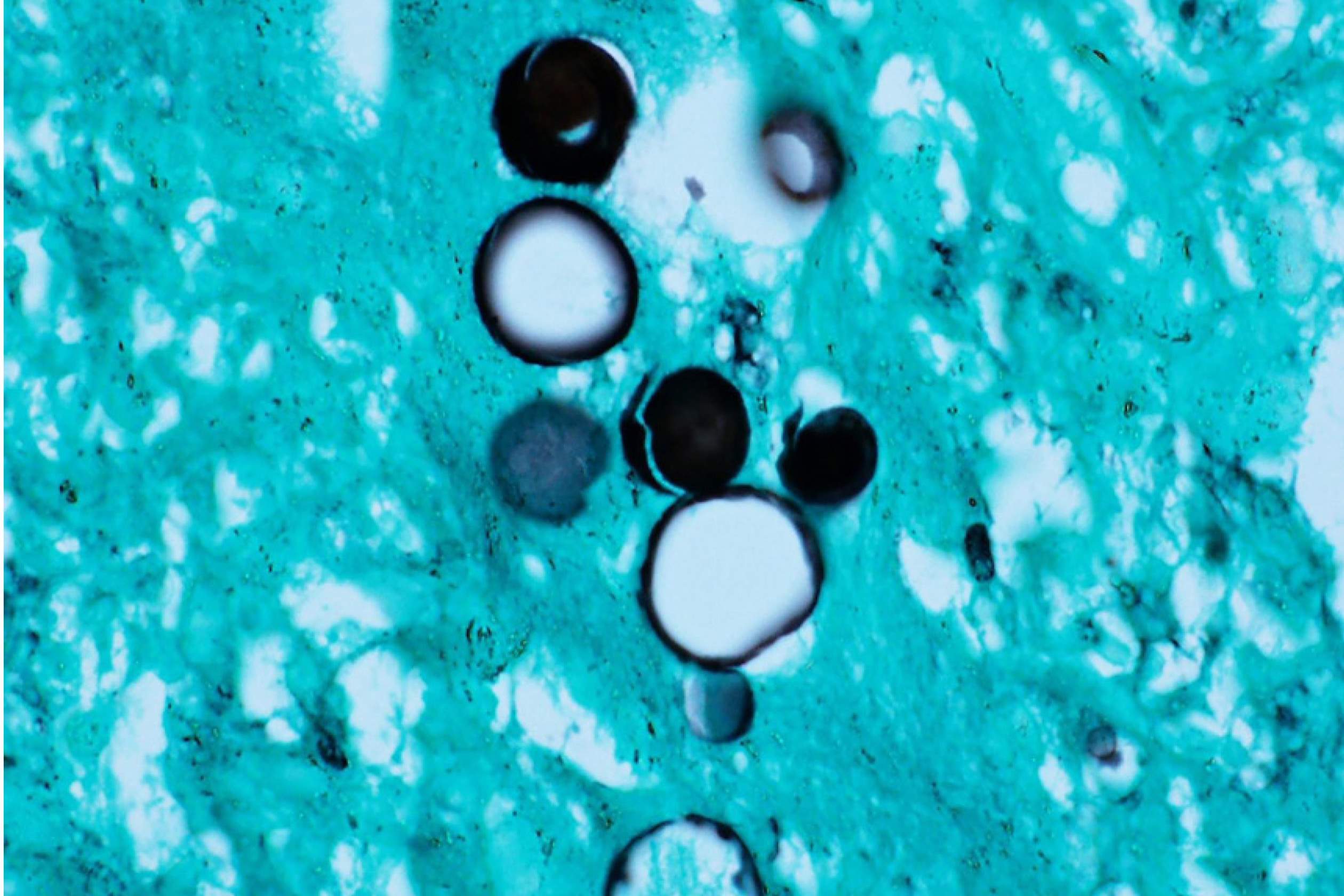
Biopsy is crucial for diagnosis. Tissue samples are examined under a microscope to identify the fungus.
Treatment and Prognosis
Effective treatment options and understanding the prognosis are vital for managing PCM.
-
Antifungal medications are the primary treatment. Drugs like itraconazole and amphotericin B are commonly used.
-
Treatment duration can be lengthy. Patients may need to take antifungal medications for several months to years.
-
Early treatment improves outcomes. Prompt medical intervention can prevent complications and improve survival rates.
-
Relapses can occur. Even after successful treatment, some patients may experience a recurrence of symptoms.
-
Supportive care is essential. Nutritional support and management of secondary infections are important aspects of treatment.
Risk Factors and Prevention
Knowing the risk factors and preventive measures can help reduce the incidence of PCM.
-
Living in endemic areas increases risk. People residing in rural parts of Latin America are more susceptible.
-
Occupational exposure is a significant risk factor. Jobs involving soil disturbance, like farming and construction, elevate the risk.
-
Smoking can worsen the disease. Smokers are more likely to develop severe forms of PCM.
-
Poor nutrition can increase susceptibility. Malnourished individuals have a weakened immune system, making them more prone to infection.
-
Preventive measures are limited. Avoiding soil exposure and wearing protective masks can reduce risk but are not foolproof.
Historical and Scientific Insights
The history and scientific discoveries related to PCM offer fascinating insights into this disease.
-
PCM was first described in 1908. Brazilian physician Adolfo Lutz identified the disease.
-
The fungus was initially named Paracoccidioides brasiliensis. Recent studies have identified multiple species within the genus.
-
PCM is also known as South American blastomycosis. This name reflects its geographic prevalence.
-
Research is ongoing to develop a vaccine. Scientists are working on immunization strategies to prevent PCM.
-
Genetic studies are shedding light on the fungus. Understanding the genetic makeup of Paracoccidioides can help in developing targeted treatments.
Impact on Public Health
The broader impact of PCM on public health highlights the importance of awareness and research.
-
PCM is a neglected tropical disease. It receives less attention and funding compared to other infectious diseases.
-
The economic burden is significant. Treatment costs and loss of productivity due to illness affect communities and healthcare systems.
-
Public health campaigns are needed. Raising awareness and educating at-risk populations can help in early detection and prevention.
-
PCM can co-exist with other diseases. Patients with tuberculosis or HIV are at higher risk of developing PCM.
-
Surveillance programs are crucial. Monitoring and reporting cases can help in understanding the disease's spread and impact.
Interesting Facts and Trivia
Some lesser-known facts and trivia about PCM add to the understanding of this complex disease.
-
PCM can affect animals. Cases have been reported in dogs and armadillos.
-
The fungus can survive in various environments. It thrives in both humid and dry conditions, making it adaptable.
-
PCM has different clinical forms. The acute form affects children and young adults, while the chronic form is more common in adults.
-
The disease can mimic other conditions. PCM is often misdiagnosed as cancer or other fungal infections.
-
PCM can cause adrenal insufficiency. The fungus can infect the adrenal glands, leading to hormonal imbalances.
Future Directions and Research
Ongoing research and future directions in PCM offer hope for better management and treatment.
-
New antifungal drugs are being developed. Researchers are working on more effective and less toxic medications.
-
Molecular diagnostics are improving. Advanced techniques can detect the fungus more accurately and quickly.
-
Understanding host immunity is key. Studying how the immune system responds to Paracoccidioides can lead to better treatments.
-
Environmental studies are important. Identifying the ecological niches of the fungus can help in predicting and preventing outbreaks.
-
Collaborative research is essential. International cooperation among scientists and healthcare providers can accelerate progress in combating PCM.
Final Thoughts on Paracoccidioidomycosis
Paracoccidioidomycosis, a fungal infection primarily found in Latin America, affects many people, especially those in rural areas. Understanding its symptoms, such as persistent cough, fever, and weight loss, can lead to early diagnosis and treatment. Farmers and others working in soil-rich environments should take precautions to avoid inhaling the spores.
Treatment usually involves antifungal medications, which can be effective if started early. Awareness and education about this disease are crucial in reducing its impact. By sharing knowledge and promoting preventive measures, communities can better protect themselves.
Remember, if you or someone you know shows symptoms, seek medical advice promptly. Early intervention can make a significant difference. Stay informed, stay safe, and help spread the word about paracoccidioidomycosis. Knowledge is power in the fight against this disease.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
