Inclusion conjunctivitis is a common eye infection caused by the bacterium Chlamydia trachomatis. This condition affects both adults and infants, leading to redness, discharge, and discomfort in the eyes. But what exactly causes inclusion conjunctivitis, and how can it be treated? Understanding the symptoms and treatment options is crucial for managing this infection effectively. In this blog post, we will explore 40 facts about inclusion conjunctivitis, shedding light on its causes, symptoms, and treatment methods. Whether you're a parent concerned about your child's eye health or an adult experiencing eye irritation, this guide will provide valuable insights to help you navigate this condition.
Key Takeaways:
- Inclusion conjunctivitis is caused by Chlamydia trachomatis and can affect both newborns and adults, leading to red, swollen eyes and discharge. Early diagnosis and treatment are crucial to prevent complications.
- Preventing inclusion conjunctivitis involves prenatal screening, safe sexual practices, hygiene, and prompt treatment. Awareness and education play a key role in reducing the global impact of this eye infection.
What is Inclusion Conjunctivitis?
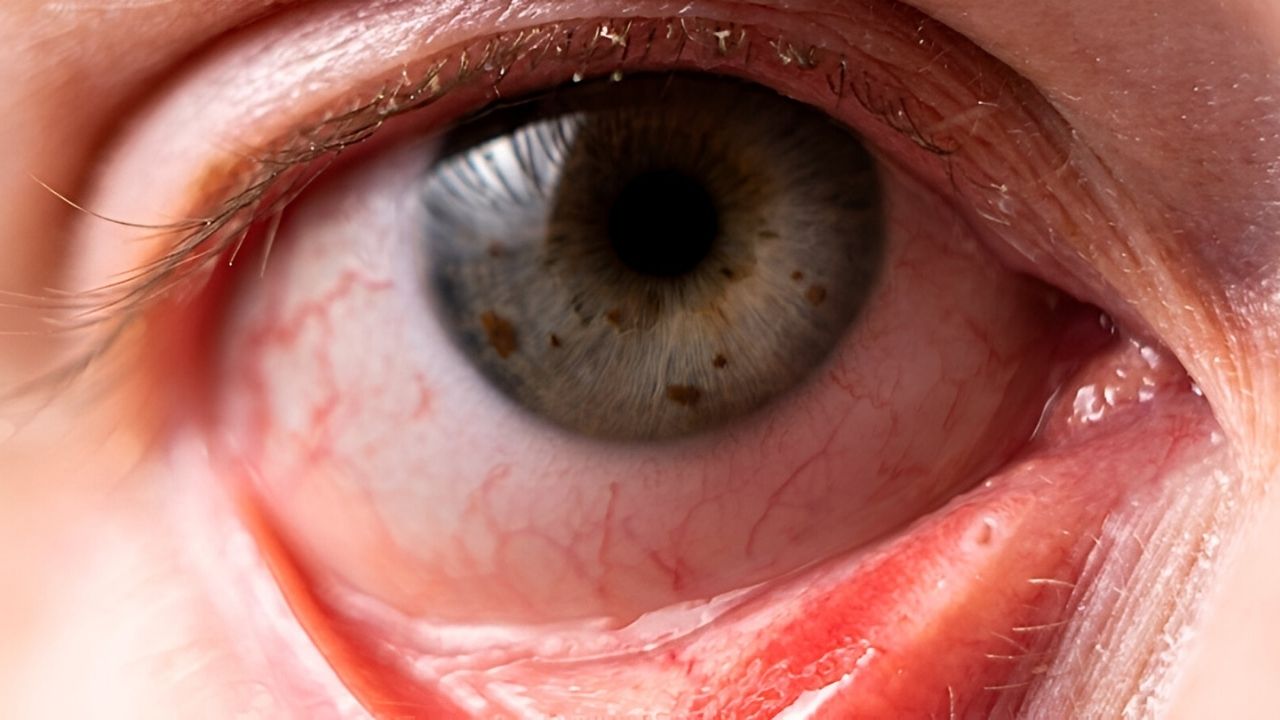
Inclusion conjunctivitis is an eye infection caused by the bacterium Chlamydia trachomatis. It primarily affects the conjunctiva, the thin membrane covering the white part of the eye and the inner surface of the eyelids. Let's dive into some fascinating facts about this condition.
-
Caused by Chlamydia trachomatis: This bacterium is the same one responsible for the sexually transmitted infection chlamydia.
-
Affects Newborns and Adults: Newborns can contract it during birth if the mother has a chlamydia infection. Adults can get it through direct contact with infected secretions.
-
Symptoms in Newborns: Symptoms in newborns usually appear within 5 to 12 days after birth and include red, swollen eyes with discharge.
-
Symptoms in Adults: Adults may experience redness, irritation, and discharge in one or both eyes, often accompanied by swollen lymph nodes near the ears.
-
Not the Same as Pink Eye: While it shares some symptoms with viral or bacterial conjunctivitis (pink eye), inclusion conjunctivitis is specifically caused by Chlamydia trachomatis.
How is Inclusion Conjunctivitis Diagnosed?
Diagnosis involves a combination of clinical examination and laboratory tests. Here are some key facts about the diagnostic process.
-
Eye Swab Test: A sample of the discharge from the eye is taken and tested for the presence of Chlamydia trachomatis.
-
Polymerase Chain Reaction (PCR): This highly sensitive test can detect the genetic material of Chlamydia trachomatis in the eye swab sample.
-
Fluorescent Antibody Staining: This technique uses fluorescent dyes to detect chlamydia bacteria in the sample.
-
Culture Test: Although less commonly used, culturing the bacteria from the eye swab can confirm the diagnosis.
-
Clinical Examination: Doctors look for characteristic signs like redness, swelling, and discharge to make a preliminary diagnosis.
Treatment Options for Inclusion Conjunctivitis
Effective treatment is crucial to prevent complications and spread. Here are some treatment facts.
-
Antibiotic Eye Drops: These are often prescribed to eliminate the infection locally.
-
Oral Antibiotics: In some cases, oral antibiotics like azithromycin or doxycycline are necessary to treat the infection systemically.
-
Treatment for Newborns: Newborns are usually treated with oral erythromycin to ensure the infection is fully cleared.
-
Follow-Up Care: Regular follow-up visits are essential to ensure the infection has been completely eradicated.
-
Treating Sexual Partners: Sexual partners should also be treated to prevent reinfection and further spread.
Prevention of Inclusion Conjunctivitis
Preventive measures can significantly reduce the risk of contracting or spreading this infection. Here are some important prevention facts.
-
Prenatal Screening: Pregnant women should be screened for chlamydia to prevent transmission to the newborn.
-
Safe Sexual Practices: Using condoms and having regular STI screenings can reduce the risk of contracting chlamydia.
-
Hygiene Practices: Washing hands frequently and avoiding touching the eyes can help prevent the spread of infection.
-
Avoid Sharing Personal Items: Items like towels and makeup should not be shared to prevent transmission.
-
Prompt Treatment: Early treatment of chlamydia infections can prevent complications like inclusion conjunctivitis.
Complications of Untreated Inclusion Conjunctivitis
If left untreated, inclusion conjunctivitis can lead to several complications. Here are some critical facts about potential complications.
-
Chronic Conjunctivitis: The infection can become chronic, leading to persistent symptoms and discomfort.
-
Corneal Ulcers: Severe cases can cause ulcers on the cornea, potentially leading to vision loss.
-
Scarring: Repeated infections can cause scarring of the conjunctiva, affecting eye movement and comfort.
-
Spread of Infection: The bacteria can spread to other parts of the body, causing more severe health issues.
-
Increased Risk of Other STIs: Having chlamydia increases the risk of contracting other sexually transmitted infections.
Global Impact of Inclusion Conjunctivitis
Inclusion conjunctivitis affects people worldwide, with varying prevalence and impact. Here are some global facts.
-
Common in Developing Countries: Higher rates are seen in areas with limited access to healthcare and prenatal screening.
-
Neonatal Conjunctivitis Rates: In some regions, up to 30% of newborns with conjunctivitis have inclusion conjunctivitis.
-
Public Health Efforts: Global health organizations are working to reduce the prevalence through education and screening programs.
-
Antibiotic Resistance: Emerging antibiotic resistance is a growing concern, making treatment more challenging.
-
Awareness Campaigns: Increased awareness and education can help reduce the incidence and spread of the infection.
Historical Context of Inclusion Conjunctivitis
Understanding the history of inclusion conjunctivitis provides insight into how it has been managed over time. Here are some historical facts.
-
First Described in the 19th Century: The condition was first documented in the late 1800s.
-
Early Treatments: Initial treatments included silver nitrate drops, which were later found to be less effective than antibiotics.
-
Discovery of Chlamydia trachomatis: The bacterium was identified as the cause of the infection in the mid-20th century.
-
Advancements in Diagnostics: Modern diagnostic techniques like PCR have revolutionized the detection and management of the infection.
-
Evolution of Antibiotics: The development of effective antibiotics has significantly improved treatment outcomes.
Interesting Facts About Inclusion Conjunctivitis
Here are some intriguing and lesser-known facts about inclusion conjunctivitis.
-
Not Just a Human Problem: Some animals, like koalas, can also suffer from chlamydia infections, including conjunctivitis.
-
Eye Infections and STIs: Inclusion conjunctivitis highlights the connection between eye infections and sexually transmitted infections.
-
Symptom Variability: Symptoms can vary widely, from mild irritation to severe pain and vision problems.
-
Self-Limiting in Some Cases: In rare instances, the infection may resolve on its own without treatment, though this is not recommended.
-
Research Continues: Ongoing research aims to develop better treatments and preventive measures for inclusion conjunctivitis.
Final Thoughts on Inclusion Conjunctivitis
Inclusion conjunctivitis, caused by Chlamydia trachomatis, is more common than you might think. It's crucial to recognize the symptoms early—redness, discharge, and irritation—to prevent complications. This condition can affect anyone, but newborns and sexually active adults are at higher risk. Treatment usually involves antibiotics, which are highly effective when prescribed correctly.
Preventive measures, like practicing safe sex and ensuring proper prenatal care, can significantly reduce the risk. Regular eye check-ups also play a vital role in early detection and management. Understanding these facts empowers you to take proactive steps in maintaining eye health.
Stay informed, stay vigilant, and don't hesitate to seek medical advice if you notice any symptoms. Your eyes are invaluable, and taking care of them should always be a priority.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
