Inclusion-cell disease, also known as I-cell disease, is a rare genetic disorder that affects the body's ability to break down certain molecules. This condition is caused by a deficiency in an enzyme called N-acetylglucosamine-1-phosphotransferase. Without this enzyme, cells can't properly dispose of waste, leading to a buildup of substances that can damage tissues and organs. Symptoms often appear in infancy and can include developmental delays, skeletal abnormalities, and heart problems. Life expectancy for individuals with I-cell disease is typically shortened, with many not surviving past childhood. Understanding this disease is crucial for early diagnosis and management.
Key Takeaways:
- Inclusion-Cell Disease is a rare genetic disorder affecting the body's ability to break down certain fats and carbohydrates, leading to various health issues. Early recognition and supportive therapies are crucial for managing symptoms and improving quality of life.
- Families affected by Inclusion-Cell Disease can benefit from genetic counseling, support groups, and ongoing research offering hope for better treatments. Collaboration and awareness play a vital role in finding solutions for this rare disease.
What is Inclusion-Cell Disease?
Inclusion-Cell Disease, also known as I-Cell Disease or Mucolipidosis II, is a rare genetic disorder. It affects the body's ability to break down certain fats and carbohydrates. This leads to the accumulation of these substances in cells, causing various health issues.
-
Inclusion-Cell Disease is a lysosomal storage disorder. Lysosomes are cell structures that digest and recycle different molecules. In I-Cell Disease, lysosomes can't break down certain substances, leading to their buildup.
-
The disease is inherited in an autosomal recessive manner. This means a child must inherit two defective genes, one from each parent, to develop the condition.
-
Symptoms usually appear in infancy. Babies with I-Cell Disease may show signs like developmental delays, abnormal facial features, and skeletal abnormalities.
-
It is caused by mutations in the GNPTAB gene. This gene provides instructions for making an enzyme crucial for lysosomal function.
-
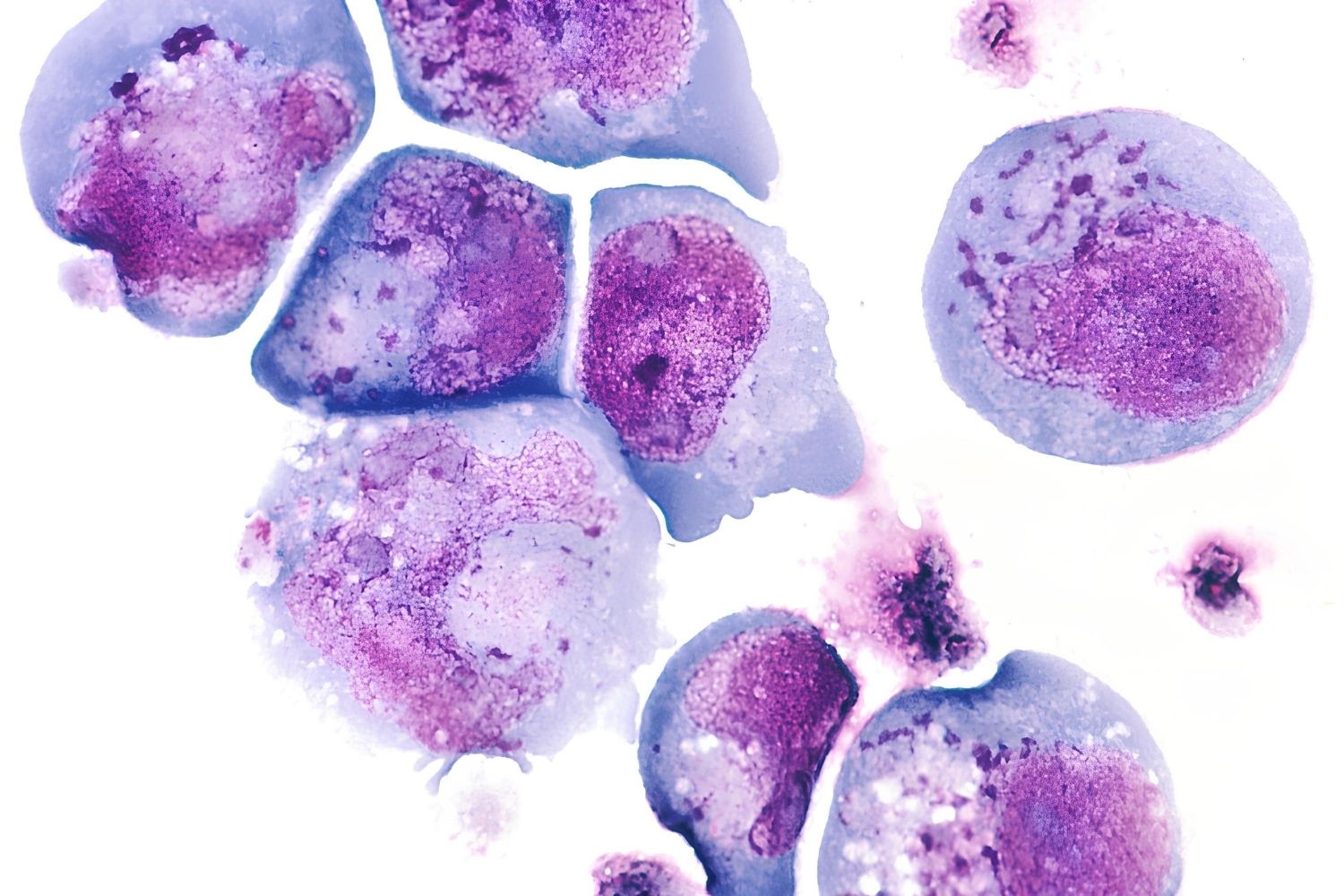
The disease is named for the "inclusion cells" seen under a microscope. These cells contain abnormal storage materials, giving the disease its name.
Symptoms and Diagnosis
Recognizing the symptoms early can help manage the disease better. Diagnosis often involves a combination of clinical evaluation and genetic testing.
-
Common symptoms include coarse facial features. These may include a flat nasal bridge, thick lips, and an enlarged tongue.
-
Skeletal abnormalities are prevalent. These can include short stature, joint stiffness, and curvature of the spine.
-
Developmental delays are a significant concern. Children with I-Cell Disease often experience delayed motor skills and intellectual disabilities.
-
Heart problems are also common. Many patients develop heart valve abnormalities, which can lead to heart failure.
-
Respiratory issues frequently occur. These can include frequent lung infections and breathing difficulties.
-
Diagnosis often involves enzyme assays. These tests measure the activity of specific enzymes in blood or tissue samples.
-
Genetic testing confirms the diagnosis. Identifying mutations in the GNPTAB gene can provide a definitive diagnosis.
Treatment and Management
While there is no cure for Inclusion-Cell Disease, various treatments can help manage symptoms and improve quality of life.
-
Enzyme replacement therapy is not effective. Unlike some other lysosomal storage disorders, enzyme replacement therapy doesn't work for I-Cell Disease.
-
Supportive care is crucial. This includes physical therapy, occupational therapy, and speech therapy to help manage developmental delays and improve quality of life.
-
Regular monitoring of heart function is essential. This helps detect and manage heart valve abnormalities early.
-
Respiratory support may be needed. Some patients require breathing assistance, especially during infections.
-
Surgical interventions can help with skeletal issues. Procedures to correct spinal curvature or joint problems may be necessary.
-
Nutritional support is important. Ensuring proper nutrition can help manage growth and development issues.
Prognosis and Life Expectancy
Understanding the prognosis and life expectancy can help families prepare and plan for the future.
-
Life expectancy is significantly reduced. Most children with I-Cell Disease do not survive beyond early childhood.
-
Quality of life can vary. With proper management, some children can achieve a better quality of life despite their limitations.
-
Early intervention is key. Starting supportive therapies early can improve outcomes and help manage symptoms more effectively.
-
Research is ongoing. Scientists are continually studying I-Cell Disease to find better treatments and potentially a cure.
Genetic Counseling and Family Planning
Genetic counseling can provide valuable information for families affected by Inclusion-Cell Disease.
-
Carrier testing is available. Parents can be tested to see if they carry the defective gene.
-
Prenatal testing can detect the disease early. This allows families to make informed decisions about their pregnancy.
-
Genetic counseling helps families understand risks. Counselors can explain the likelihood of passing the disease to future children.
-
Family planning options are available. These may include in vitro fertilization with genetic screening to ensure healthy embryos.
Support and Resources
Finding support and resources can make a significant difference for families dealing with Inclusion-Cell Disease.
-
Support groups offer emotional help. Connecting with other families facing similar challenges can provide comfort and advice.
-
Educational resources are available. Many organizations provide information about the disease and how to manage it.
-
Financial assistance programs exist. These can help cover the costs of medical care and supportive therapies.
-
Advocacy organizations work to raise awareness. These groups strive to improve research funding and support for affected families.
Research and Future Directions
Ongoing research offers hope for better treatments and possibly a cure for Inclusion-Cell Disease.
-
Gene therapy is being explored. Scientists are investigating ways to correct the genetic defect causing the disease.
-
Stem cell research shows promise. Using stem cells to replace defective cells could offer a potential treatment.
-
Clinical trials are ongoing. New treatments are being tested to see if they can improve symptoms or slow disease progression.
-
International collaboration is key. Researchers around the world are working together to find solutions for I-Cell Disease.
-
Patient registries help track progress. These databases collect information about patients to help researchers understand the disease better.
-
Advances in technology aid research. New tools and techniques are making it easier to study the genetic and biochemical aspects of the disease.
-
Public awareness campaigns are important. Raising awareness can lead to more funding and support for research efforts.
-
Advocacy for rare diseases is growing. More attention is being given to rare diseases like I-Cell Disease, leading to increased research efforts.
-
Collaboration with pharmaceutical companies is vital. Working with drug companies can help bring new treatments to market faster.
-
Hope for the future remains strong. With ongoing research and support, there is hope for better treatments and a cure for Inclusion-Cell Disease.
Final Thoughts on Inclusion-Cell Disease
Inclusion-Cell Disease, also known as I-Cell Disease, is a rare genetic disorder that affects many parts of the body. It’s caused by mutations in the GNPTAB gene, leading to a buildup of certain substances in cells. This buildup causes cells to malfunction, leading to severe developmental issues. Symptoms often appear in infancy and can include growth delays, skeletal abnormalities, and heart problems.
There’s no cure yet, but treatments focus on managing symptoms and improving quality of life. Early diagnosis is crucial for better outcomes. Genetic counseling can help families understand the risks and implications.
Raising awareness about I-Cell Disease is vital. It helps in early detection and supports research for better treatments. If you suspect any symptoms, consult a healthcare professional. Knowledge and early intervention can make a significant difference.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
