Primary Agammaglobulinemia is a rare immune disorder where the body can't produce enough antibodies, leaving individuals vulnerable to infections. This condition, often diagnosed in childhood, stems from genetic mutations affecting B cells, the immune system's antibody factories. Symptoms include frequent respiratory infections, chronic diarrhea, and skin infections. Diagnosis involves blood tests revealing low antibody levels and genetic testing. Treatment typically includes regular immunoglobulin replacement therapy to boost the immune system. Living with Primary Agammaglobulinemia requires careful management to avoid infections and maintain health. Understanding this condition helps in providing better care and support for those affected.
Key Takeaways:
- Primary Agammaglobulinemia is a rare genetic disorder that weakens the immune system, making people more prone to infections. Treatment involves regular immunoglobulin therapy and careful management to stay healthy.
- Living with Primary Agammaglobulinemia requires extra precautions to prevent infections, including frequent medical check-ups, avoiding live vaccines, and maintaining a balanced diet and exercise routine.
What is Primary Agammaglobulinemia?
Primary Agammaglobulinemia is a rare genetic disorder affecting the immune system. It leads to a significant reduction in the production of antibodies, making individuals more susceptible to infections. Here are some fascinating facts about this condition.
-
Genetic Origin: Primary Agammaglobulinemia is usually inherited in an X-linked recessive pattern, meaning it primarily affects males.
-
Discovery: The condition was first described by Dr. Ogden Bruton in 1952, hence it is sometimes called Bruton’s Agammaglobulinemia.
-
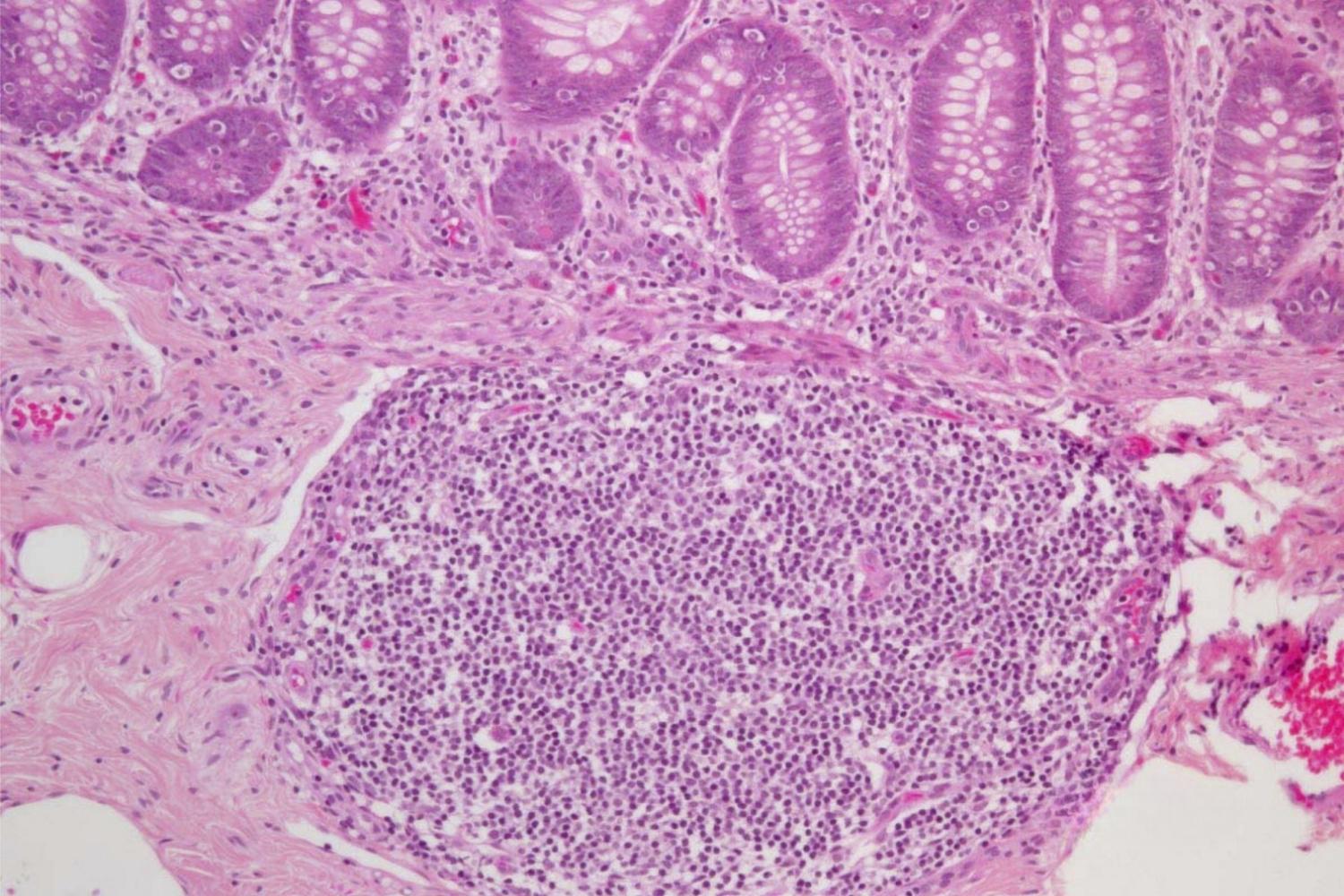
B Cells: Individuals with this disorder have very few or no B cells, which are crucial for producing antibodies.
-
Infections: People with Primary Agammaglobulinemia are prone to recurrent bacterial infections, especially in the respiratory and gastrointestinal tracts.
-
Diagnosis Age: Most cases are diagnosed in early childhood, typically between six months and two years of age.
-
Symptoms: Common symptoms include frequent ear infections, sinusitis, pneumonia, and skin infections.
-
Antibody Levels: Blood tests in affected individuals show extremely low levels of all types of immunoglobulins (IgG, IgA, IgM).
-
Genetic Testing: Diagnosis can be confirmed through genetic testing, identifying mutations in the BTK gene.
-
Carrier Mothers: Mothers who are carriers of the defective gene have a 50% chance of passing it to their sons.
-
Treatment: Regular immunoglobulin replacement therapy is the primary treatment, helping to boost the immune system.
How Does Primary Agammaglobulinemia Affect Daily Life?
Living with Primary Agammaglobulinemia requires careful management to prevent infections and maintain health. Here are some ways it impacts daily life.
-
Frequent Medical Visits: Regular check-ups with immunologists are necessary to monitor health and adjust treatments.
-
Infection Prevention: Individuals must take extra precautions to avoid infections, such as practicing good hygiene and avoiding crowded places.
-
Vaccinations: Live vaccines are generally avoided, as they can cause serious complications in people with weakened immune systems.
-
Antibiotics: Prophylactic antibiotics may be prescribed to prevent bacterial infections.
-
Diet and Nutrition: A balanced diet rich in vitamins and minerals supports overall health and immune function.
-
Exercise: Regular, moderate exercise can help strengthen the body and improve overall well-being.
-
Mental Health: Coping with a chronic illness can be challenging, so mental health support is important.
-
Education: Schools need to be informed about the condition to provide a safe environment and accommodate medical needs.
-
Social Life: Social interactions may be limited to reduce infection risk, but staying connected with friends and family is crucial.
-
Emergency Plan: Having a plan in place for medical emergencies ensures quick and effective response to health crises.
Advances in Research and Treatment
Research continues to improve the understanding and management of Primary Agammaglobulinemia. Here are some recent advancements.
-
Gene Therapy: Experimental gene therapy aims to correct the defective BTK gene, offering potential long-term solutions.
-
New Medications: Development of new immunoglobulin products and delivery methods enhances treatment options.
-
Clinical Trials: Ongoing clinical trials test innovative treatments and therapies to improve patient outcomes.
-
Personalized Medicine: Advances in genetic research allow for more personalized treatment plans based on individual genetic profiles.
-
Stem Cell Research: Investigating the use of stem cells to regenerate healthy immune cells shows promise.
-
Global Collaboration: International research collaborations accelerate the discovery of new treatments and improve patient care.
-
Patient Registries: Establishing patient registries helps track the condition’s progression and effectiveness of treatments.
-
Awareness Campaigns: Increased awareness and education about Primary Agammaglobulinemia lead to earlier diagnosis and better management.
-
Support Groups: Online and in-person support groups provide valuable resources and community for affected individuals and families.
-
Future Outlook: With ongoing research and medical advancements, the future looks hopeful for those living with Primary Agammaglobulinemia.
Final Thoughts on Primary Agammaglobulinemia
Primary Agammaglobulinemia, a rare immune disorder, affects many lives. Understanding its symptoms, causes, and treatments can make a huge difference. Early diagnosis is crucial for managing this condition effectively. Regular check-ups, immunoglobulin replacement therapy, and staying informed about new treatments are key steps. Support from healthcare professionals and patient communities can provide much-needed guidance and comfort. Awareness and education about Primary Agammaglobulinemia help in reducing stigma and improving the quality of life for those affected. By staying proactive and informed, individuals and families can navigate the challenges of this condition more effectively. Remember, knowledge is power when dealing with any health issue. Stay curious, stay informed, and support each other in the journey towards better health.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
