Palmitoyl-Protein Thioesterase Deficiency (PPT1 deficiency) is a rare genetic disorder that affects the nervous system. This condition, also known as Infantile Neuronal Ceroid Lipofuscinosis (INCL), primarily impacts young children. Symptoms often appear between six months and two years of age. These include developmental delays, seizures, and vision loss. The disorder results from mutations in the PPT1 gene, leading to the buildup of harmful substances in cells. This accumulation damages brain cells, causing progressive neurological decline. While there is no cure, treatments focus on managing symptoms and improving quality of life. Understanding PPT1 deficiency can help families and medical professionals provide better care and support.
Key Takeaways:
- Palmitoyl-Protein Thioesterase Deficiency (PPTD) is a rare genetic disorder affecting the nervous system, causing symptoms like seizures and vision loss, with no cure currently available.
- Early diagnosis and supportive care are crucial for managing PPTD, with ongoing research offering hope for better treatments and potential cures in the future.
What is Palmitoyl-Protein Thioesterase Deficiency?
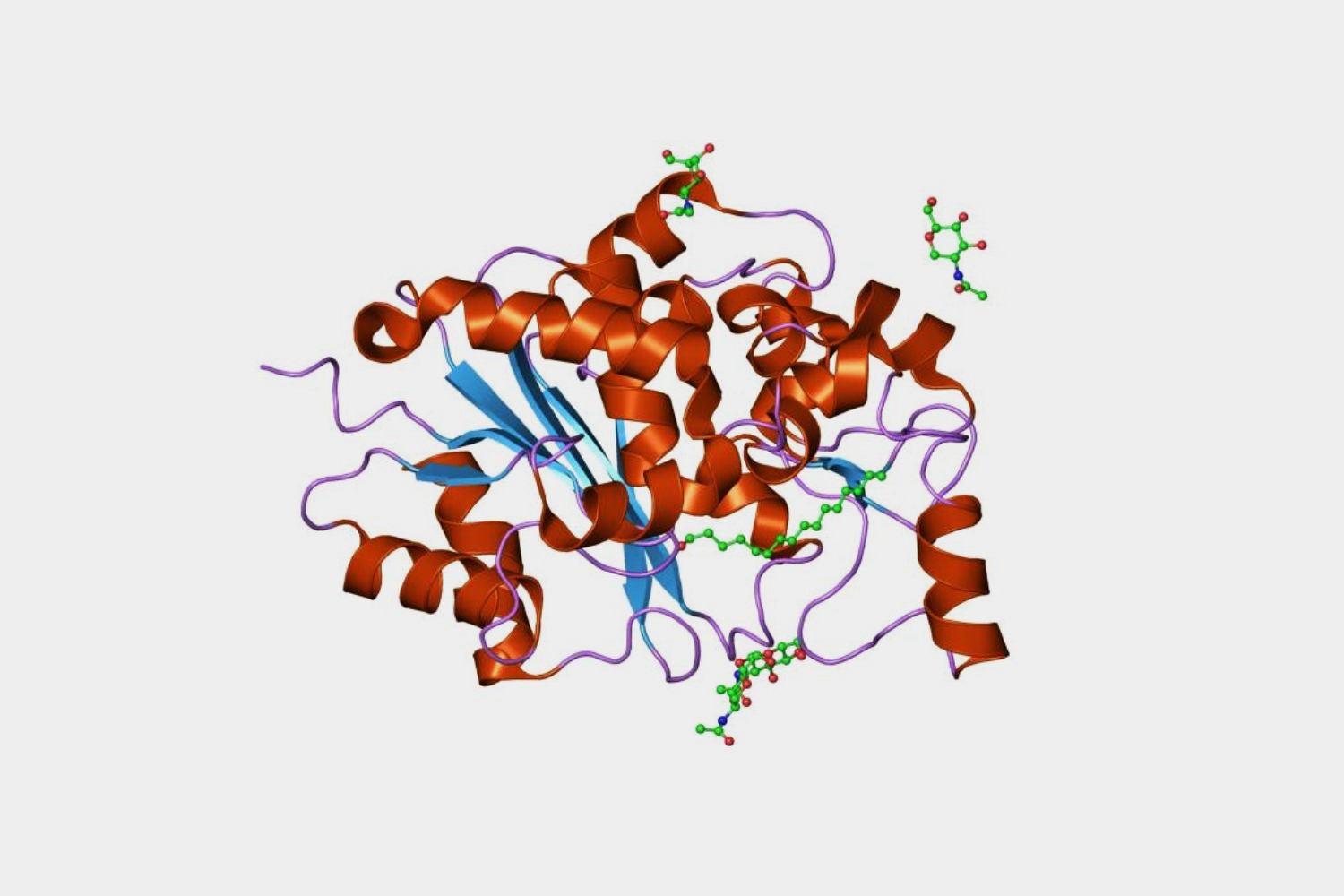
Palmitoyl-Protein Thioesterase Deficiency (PPTD) is a rare genetic disorder that affects the nervous system. It is caused by mutations in the CLN1 gene, leading to a deficiency in the enzyme palmitoyl-protein thioesterase 1 (PPT1). This enzyme is crucial for breaking down certain fatty acids in the body.
- PPTD is also known as Infantile Neuronal Ceroid Lipofuscinosis (INCL).
- The disorder is inherited in an autosomal recessive pattern.
- Symptoms usually appear between 6 months and 2 years of age.
- Common early symptoms include developmental delay and seizures.
- Vision loss is a hallmark of the disease, often occurring by age 2.
Genetic Basis of PPTD
Understanding the genetic foundation of PPTD helps in diagnosing and potentially treating the disorder. The CLN1 gene mutation disrupts normal cellular functions.
- The CLN1 gene provides instructions for making the PPT1 enzyme.
- Mutations in CLN1 lead to the accumulation of lipofuscins, harmful substances in cells.
- Over 70 different mutations in the CLN1 gene have been identified.
- Genetic testing can confirm a diagnosis of PPTD.
- Carrier testing is available for family members of affected individuals.
Symptoms and Progression
PPTD symptoms worsen over time, severely impacting the quality of life. Early detection can help manage symptoms more effectively.
- Motor skills decline rapidly, leading to loss of mobility.
- Affected children often develop muscle stiffness and rigidity.
- Speech and language skills deteriorate as the disease progresses.
- Feeding difficulties and swallowing problems are common in later stages.
- Life expectancy is significantly reduced, often not beyond early childhood.
Diagnosis and Screening
Early and accurate diagnosis is crucial for managing PPTD. Various tests and screenings are used to identify the disorder.
- Enzyme activity tests measure the function of PPT1 in blood or skin cells.
- MRI scans can show brain abnormalities typical of PPTD.
- Electroencephalograms (EEGs) detect abnormal brain activity.
- Ophthalmologic exams assess vision loss and retinal degeneration.
- Prenatal testing is available for at-risk pregnancies.
Treatment and Management
While there is no cure for PPTD, treatments focus on managing symptoms and improving quality of life. Supportive care is essential for affected individuals.
- Anticonvulsant medications help control seizures.
- Physical therapy can maintain mobility and muscle function.
- Speech therapy supports communication skills for as long as possible.
- Nutritional support is vital due to feeding difficulties.
- Palliative care provides comfort and support in advanced stages.
Research and Future Directions
Ongoing research aims to find better treatments and, ultimately, a cure for PPTD. Advances in genetics and biotechnology offer hope for the future.
- Gene therapy is being explored as a potential treatment.
- Stem cell research may offer new avenues for regenerating damaged tissues.
- Clinical trials are testing new drugs to slow disease progression.
- Patient registries help researchers gather data and track disease patterns.
- Advocacy groups raise awareness and support families affected by PPTD.
Final Thoughts on Palmitoyl-Protein Thioesterase Deficiency
Palmitoyl-Protein Thioesterase Deficiency, also known as PPT1 deficiency, is a rare but serious condition. It affects the nervous system, leading to progressive symptoms that can be challenging for patients and their families. Early diagnosis and intervention can make a significant difference in managing the disease. While there's no cure yet, ongoing research offers hope for better treatments in the future. Understanding the genetic basis and symptoms of PPT1 deficiency helps in raising awareness and supporting those affected. If you or someone you know is dealing with this condition, connecting with support groups and medical professionals can provide valuable resources and emotional support. Knowledge is power, and staying informed about the latest developments can make a world of difference.
Frequently Asked Questions
Was this page helpful?
Our commitment to delivering trustworthy and engaging content is at the heart of what we do. Each fact on our site is contributed by real users like you, bringing a wealth of diverse insights and information. To ensure the highest standards of accuracy and reliability, our dedicated editors meticulously review each submission. This process guarantees that the facts we share are not only fascinating but also credible. Trust in our commitment to quality and authenticity as you explore and learn with us.
